Commitment, Flexibility and Multidisciplinary Teams Bring Excellence to COVID Care
Clinical Affairs | CU School of Medicine Jun 29, 2020
When news of the COVID-19 pandemic in the U.S. started to emerge, no one knew quite what to expect. But many at the School of Medicine and University of Colorado Hospital (UCH) knew that the hospital’s status as an academic medical center and quaternary care referral facility meant it would be playing a key role in responding to the pandemic in the Denver metro area.
Collaborating across Departments
As ill patients began to arrive and the numbers of cases climbed across the country, hospitalists Marisha Burden, MD, Associate Professor of Hospital Medicine and Division Head of Hospital Medicine and Kasey Bowden, MSN, FNP, AGANP, Assistant Professor of Medicine and Associate Clinical Director for the Division of Hospital Medicine, saw how the Hospital Medicine division could add support for the surge of COVID patients on the floor and in the intensive care unit.
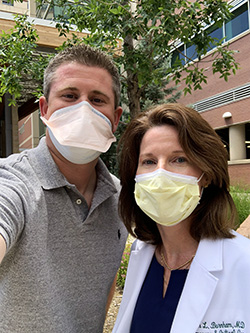
Pictured above are Kasey Bowden and Marisha Burden (l-r)
“Hospital medicine cares for about half of patients in the hospital at any given time, so we are a large division. We recognized that we had a unique ability to see a high volume of patients that other divisions just didn’t have the staff power to handle,” said Ms. Bowden. “We partnered with critical care services so hospital medicine could provide some of that critical care coverage when patient volume increased.”
The sudden surge in hospitalized and critically ill patients demanded a swift, significant response. To meet this need, leadership began meeting daily to develop a plan, and intensivists from the Departments of Medicine, Anesthesiology and Surgery worked in partnership to create a new care model.
 “It became clear that we would need a novel approach to ICU care. Patient census, acuity, space considerations and safety for patients and staff were significant hurdles,” said Jason Brainard, MD, Associate Professor of Anesthesiology. “Most of all, we wanted to focus on providing outstanding care to our patients. To do this, we created collaborative, multidisciplinary care teams that included physicians, advanced practice providers, nursing colleagues and other essential critical care partners from multiple departments.”
“It became clear that we would need a novel approach to ICU care. Patient census, acuity, space considerations and safety for patients and staff were significant hurdles,” said Jason Brainard, MD, Associate Professor of Anesthesiology. “Most of all, we wanted to focus on providing outstanding care to our patients. To do this, we created collaborative, multidisciplinary care teams that included physicians, advanced practice providers, nursing colleagues and other essential critical care partners from multiple departments.”
Overcoming Obstacles to Master a New Model of Care
Committed to excellence in patient care, the teams implemented the model without hesitation but with some trepidation, having little previous experience with such a dramatic reorganization of the usual ways to deliver care. It is rare for teams from multiple departments to provide care for one large patient population.
Pictured right are Drs. Jason Brainard and Ellen Burnham
Despite the concerns and uncertainty, both the patient outcomes and provider experience indicate that the model has been successful. “I knew our teams were capable of this level of sophisticated collaboration, but it is so rewarding to see it in action,” said Tom Gronow, Chief Operating Officer of University of Colorado Hospital. “It has been a difficult time for everyone, especially our front-line staff. But they can be proud of the innovative, high-quality care they’ve delivered every day during this pandemic. This type of collaboration is something we want to sustain into the future as we continue to navigate uncertainty.”
The model’s success is due in large part to the thoughtful planning and constant iteration that took place as the number of COVID cases continued to climb. Leadership met for many hours a day, every day, to talk about staffing plans and coverage models. They looked at what was working and what needed to be improved, and then iterated the care protocols in real time.
Data and analytics teams created dashboards that allowed for easy tracking of trends in patient counts in the ICU and on the floor. This high level of data and communication was essential, according to Ellen Burnham, MD, Professor of Medicine – Pulmonary Sciences & Critical Care and Director of UCH Hospital Medicine ICU. “We not only worked together clinically, but we also built cohesive strategies and shared clinical data algorithms and best practices constantly. These efforts helped us to adjust our plans in real time and in a data-driven way.”
With this concentrated effort, something that typically takes months of planning was implemented within days. The urgency of caring for a vulnerable patient population of very sick patients increased focus and determination at all levels, revitalizing the commitment to provide outstanding care to anyone who walks through the UCH doors.
Informing Practice with Research in Real Time
As an academic medical center, UCH had the skills and expertise needed to track the rapidly evolving knowledge base about COVID. The COVID response has included many of the components of academic medicine – research, literature review, knowledge dissemination, expert clinical care and adoption of new practices – all in a compressed timeframe.
Critical care physicians quickly put together an internal website to help providers curate and digest the overwhelming amount of COVID-related information. Providers needed just-in-time answers to a range of questions about work schedules, care protocols and safety. The department identified subject matter experts who organized and updated the information, giving teams a way to get the best, most reliable and up-to-date information.
That internal site evolved into a public-facing site with COVID patient care resources, guidelines and protocols. Academic clinicians from the Anschutz campus worked closely with colleagues in other medical centers, such as Denver Health and the VA Eastern Colorado Health System to exchange information and expertise. They also worked to share knowledge with non-academic hospitals in the northern and southern regions of the UCHealth system.
Top-Down or Bottom Up Change? Yes.
This level of coordination and collaboration would not have been possible without the strong support and coordination of leadership across the organization. In particular, leadership helped the team overcome some of the administrative hurdles that must be overcome in the highly regulated world of health care.
At the same time, Dr. Brainard is quick to point out that none of it would have been possible without the relentless commitment, ingenuity and flexibility of front-line staff, who never wavered despite the risk and stress of providing care.
The COVID crisis has eased for the time being but is far from over. As additional hospital services come back, the teams will have fewer faculty and residents to draw upon during future patient surges. The teams will need to adjust their staffing models, drawing on additional advanced practice providers to staff care teams. Fortunately, the teams now have expertise in the care of COVID patients that will make their work more efficient and their protocols more precise.
The teams also have an invaluable resource: each other. In caring for COVID patients, providers at all levels have experienced the benefits of working collaboratively to draw on the experiences and expertise of everyone to maximize the care they are able to provide. In the future, they will be able to build upon these relationships to provide better care to all patients, even after this pandemic is over.