Study Description
Shared medical appointments (SMAs) for diabetes have been shown to be an effective approach for helping patients manage their type-2 diabetes.
This important study sought to answer some questions around the best ways to deliver SMAs for primary care patients with diabetes - offering diabetes self-management education and support.
Type II Diabetes is a prevalent chronic disease with poor outcomes, and requires daily self-care, including blood glucose monitoring, following a diabetes-friendly diet, engaging in regular physical activity, and medication adherence. Patients with diabetes benefit from comprehensive diabetes self-management education (DSME) and self-management support (SMS) in primary care. Shared medical appointments (SMAs) are one way to efficiently and effectively provide DSME and SMS. SMAs can have a variety of different features, but it is not known which features are most effective for which types of patients.
Invested in Diabetes is a pragmatic, cluster randomized comparative effectiveness trial of diabetes shared medical appointments (SMAs) using patient-driven educational content delivered by multidisciplinary care teams including peer mentors, compared to SMAs with standardized content delivered by health educators. The aims are to implement patient-driven and standardized SMAs in twenty practices using patient and provide partner engagement and evidence-based implementation strategies, and to evaluate differences in patient participation in care, patient-reported outcomes (diabetes distress, self-care behaviors, quality of life), clinical outcomes, and practice-level adoption, implementation, and maintenance. Invested in Diabetes was funded by the Patient Centered Outcomes Research Institute (PCORI), and more information about Invested in Diabetes can be found at this link.
Patient and primary care clinic partners engaged in planning this study proposed a model with "diabetes' veterans" (i.e., diabetes peer mentors) who co-facilitating group visits with a variety of diabetes care professionals, and then working one-on-one with patients to help apply what they learned. The group visit curriculum should include topics on physical activity, healthy eating, taking medication, acceptance and coping, and social support, and each cohort of patients should get to select topics most relevant to them.
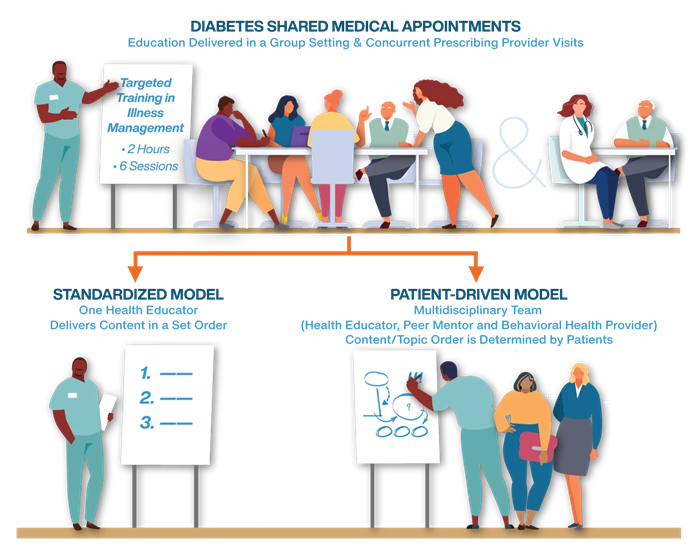
Based on feedback from our patient partners, we designed a study that compared the effectiveness of patient-driven diabetes SMAs to standardized diabetes SMAs. The curriculum used was Targeted Training for Illness Management (TTIM), a 6-session modular group intervention for chronic illness self-management, and that has been tested in diabetes.
The standardized group visit model consisted of diabetes SMAs with the full TTIM 6-session curriculum, led by a health educator. For the patient-driven SMAs, patients chose the topics and the order of sessions from the TTIM curriculum, which was delivered collaboratively by the multidisciplinary care team consisting of several professional providers (health educator, medical provider, and behavioral health provider) and a lay worker (diabetes peer mentor).
The primary patient-centered outcome, selected by patient partners, was diabetes distress. Secondary outcomes included autonomy support and diabetes self-management behaviors, clinical outcomes (hemoglobin A1c, blood pressure, and body mass index), patient reach and engagement, and practice-level value and sustainability. Patient, caregiver, and primary care practice partners as well as research collaborators were engaged in all aspects of the research. Patients and primary care practice partners informed the process of implementation of patient-driven and standardized SMAs, helped finalize the research protocol (including data collection and recruitment), and contributed to interpretation of findings and dissemination of findings, including messages that help other patients make decisions about whether or not to participate in SMAs.
Invested in Diabetes Implementation Guide.
Implementation Guide
Targeted Training in Illness Management Curriculum and Instructor Materials
Instructor Materials
The Invested in Diabetes team included experts, partners, and professionals from across the country.
Principal Investigators:
- Bethany M. Kwan (PI), CU Anschut
- Jeanette A. Waxmonsky (Co-PI), CU Anschutz
Co-Investigators:
- Russel Glasgow, PhD (Co-I), CU Anschutz
- Martha Sajatovic, MD (Co-I), Case Western Reserve University
- R. Mark Gritz, PhD (Co-I), CU Anschutz
- L Miriam Dickinson, PhD (Co-I), CU Anschutz
- Jodi S Holtrop, PhD (Co-I), CU Anschutz
- Andrea Nederveld, PhD, MPH (Co-I), CU Anschutz
- Natalie D Ritchie, PhD (Co-I), Denver Health
- Don Nease Jr., MD (Co-I), CU Anschutz
- Christina Hester, PhD (Co-I), AAFP National Research Network
- Jennifer Dailey-Vail, APRN, DNP (Co-I), CU Anschutz
Patient Partners:
- Ramona Koren
- Sharon A Trujillo
- David Downey
- Thomas Carrigan
- Barbara Clay
Professional Support:
- Dennis Gurfinkel, MPH (Study manager), CU Anschutz
- Robyn Wearner, MA, RD (practice facilitator), CU Anschutz
- Anowara Begum, MPH (research assistant), CU Anschutz
- Jack Cronin, MS (research assistant), CU Anschutz
- Julia Reedy, MA (research assistant), CU Anschutz
- Patrick Hosokawa, MS (analyst), CU Anschutz
- Jayna DeRoeck, MS (diabetes educator), Denver Health
- Kristin Cassidy, MA (research assistant), Case Western Reserve University
- Angie Lanigan, MPA, RD (research assistant), AAFP National Research Network
- Carol Gorman, BA (research assistant), CU Anschutz
- Mika Hamer, PhD (research assistant), CU Anschutz
- Johnny Williams, MPH (research assistant), CU Anschutz
- Peter Ferrarone, MA (research assistant), CU Anschutz
- Jenny Rementer, MA (former practice facilitator), CU Anschutz
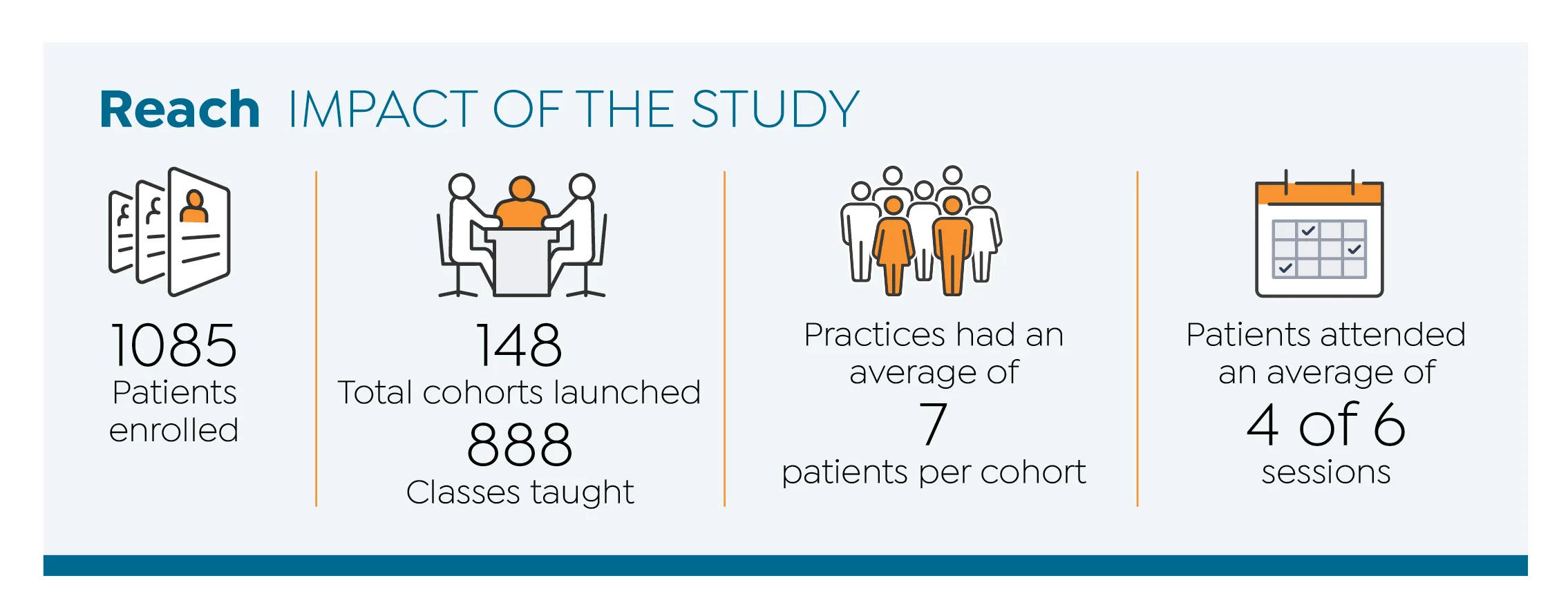
Invested in Diabetes Study Impact
Study Findings
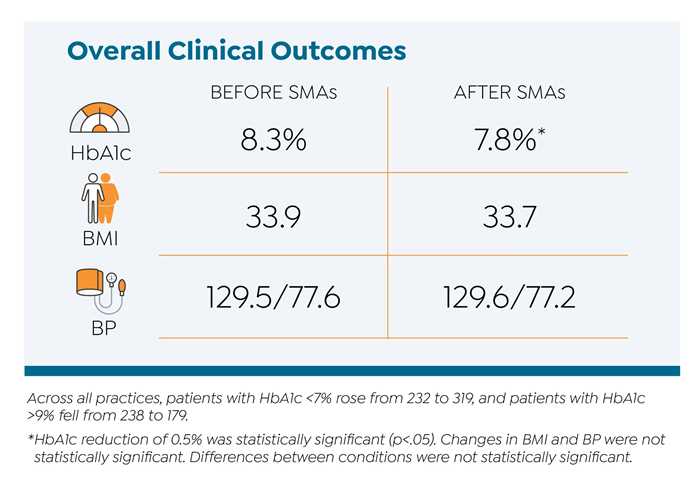
The Invested in Diabetes study compared effects of two models of diabetes SMAs — standardized and patient-driven — on patient-reported outcomes (diabetes distress, self-care behaviors) and clinical outcomes (hemoglobin A1C, blood pressure, BMI):
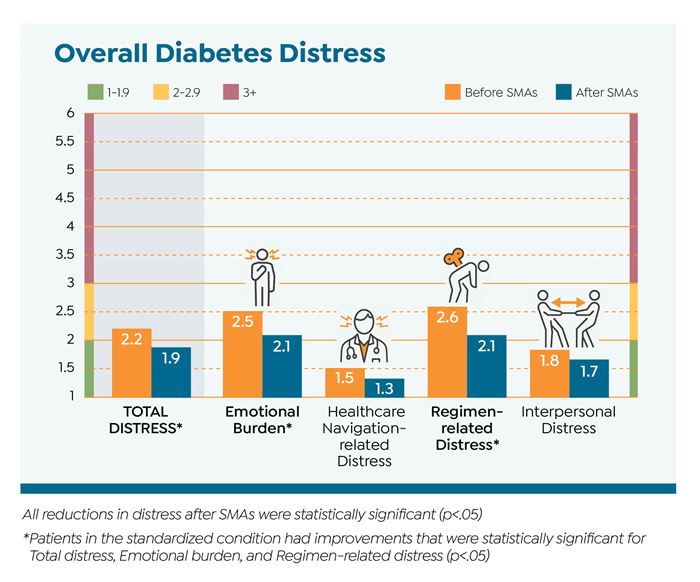
The study’s primary patient-centered outcome was diabetes distress.
Secondary outcomes included self-reported diabetes self-care behaviors, HbA1c, BMI, and blood pressure.
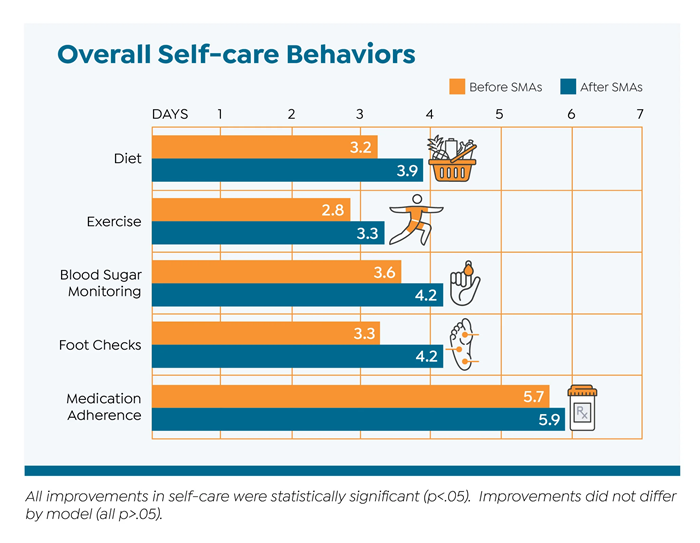
Overall, diabetes SMAs improved diabetes distress, HbA1c, self-care behaviors. Both models led to similar outcomes, although standardized SMAs led to greater improvements in diabetes distress.
Take Home Message: Patient-driven SMAs can be more expensive to set up and more challenging to coordinate and practices will have to take that into consideration when designing diabetes SMAs for their clinics.