DOM Leaders in Informatics, Quality and Systems Fellowship 
The Leaders in Informatics, Quality, and Systems (LInQS) Fellowship Program aims to develop future leaders in quality, clinical system design, learning healthcare systems, clinical informatics, and patient safety among CU Anschutz Department of Medicine fellows and faculty. This 2-year program offers didactics, mentorship, and hands-on training from expert faculty.
About the Program![]()
The didactic portion includes participation in the Quality Safety Academy, IHQSE Foundations in Healthcare Leadership Workshop, and LInQS faculty-led lectures. Participants attend regular work-in-progress meetings and tailor their experience to their career goals, with divisions protecting a portion of their time for the program.
 Deadline to submit your application is March 13th
Deadline to submit your application is March 13th
LInQS Fellows 
LInQS Fellowship Program Faculty 
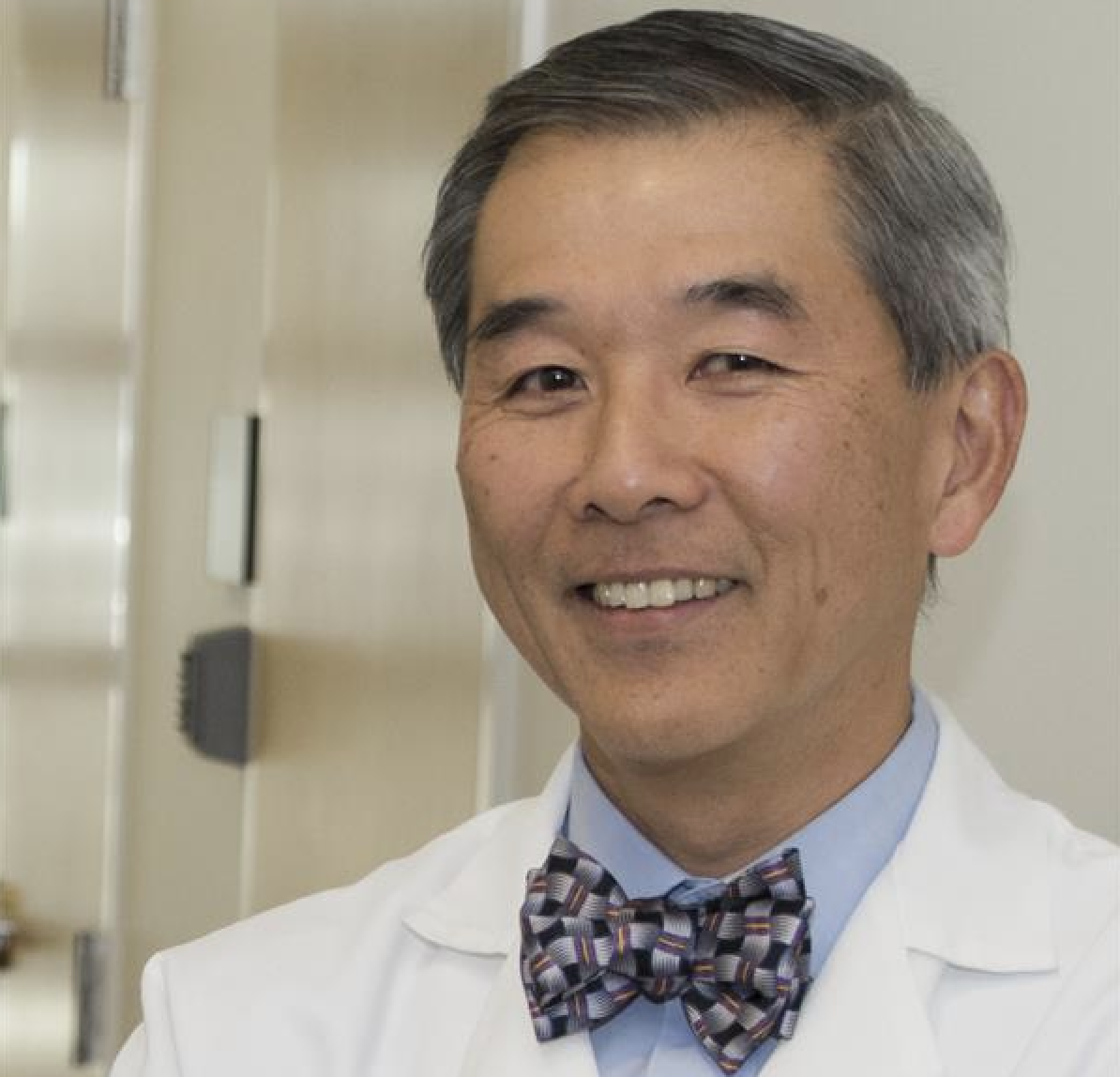
Professor, Internal Medicine
Medical Director, Office of Value Based Performance; Co-Director, D2V
Medical Director, Office of Value Based Performance; Co-Director, D2V
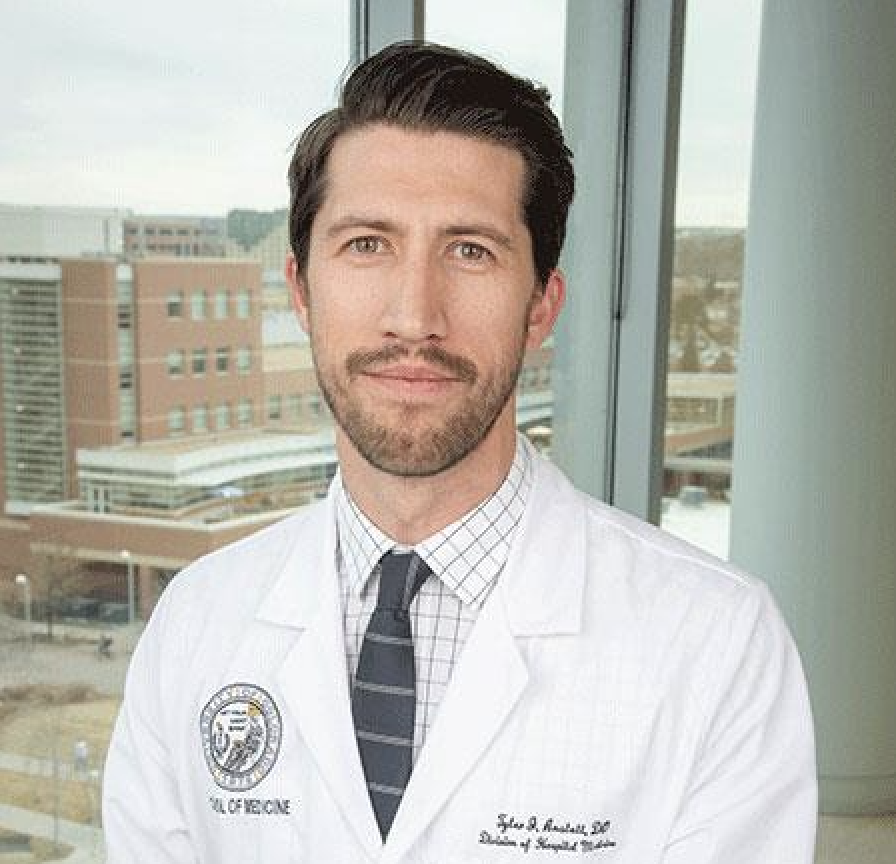
Associate Professor, Hospital Medicine
Sr. Medical Director of Informatics for UCHealth Ambulatory Services
Sr. Medical Director of Informatics for UCHealth Ambulatory Services
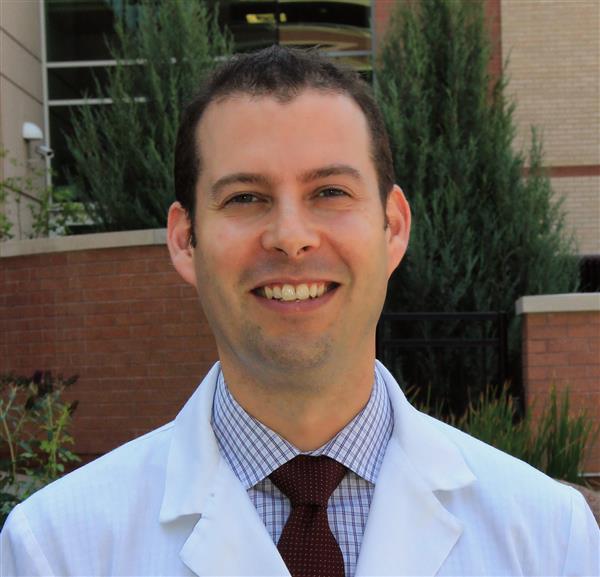
Associate Professor, Infectious Disease
Medical Director, Occupational Health
Medical Director, Occupational Health
Assistant Professor, Cardiology Clinical
Director for Inpatient Services
Quality Director, Cardiology
Associate Professor, Pulmonary, Allergy & Critical Care Medicine
Quality Director, Pulmonary, Allergy & Critical Care Medicine