.png?sfvrsn=ad9590bb_0) Curriculum
Curriculum
 The University of Colorado leads in educational innovation. Our novel 36-month curriculum is a model for the future of residency training and the creation of highly skilled, well-rounded doctors. We have developed an innovative, learner-centered residency curriculum that ensures a broad education for all housestaff yet provides multiple different curricular combinations to allow residents to tailor their training based on personal career goals. Our curriculum also balances inpatient and outpatient experiences as well as apprenticeship-based learning with non-apprenticeship experiences to make a modern doctor. Dedicated time for scholarship, quality training, subspecialty pursuits, and four overlapping and complimentary curricula round out this truly unique experience.
The University of Colorado leads in educational innovation. Our novel 36-month curriculum is a model for the future of residency training and the creation of highly skilled, well-rounded doctors. We have developed an innovative, learner-centered residency curriculum that ensures a broad education for all housestaff yet provides multiple different curricular combinations to allow residents to tailor their training based on personal career goals. Our curriculum also balances inpatient and outpatient experiences as well as apprenticeship-based learning with non-apprenticeship experiences to make a modern doctor. Dedicated time for scholarship, quality training, subspecialty pursuits, and four overlapping and complimentary curricula round out this truly unique experience.
A Matrix of Options:
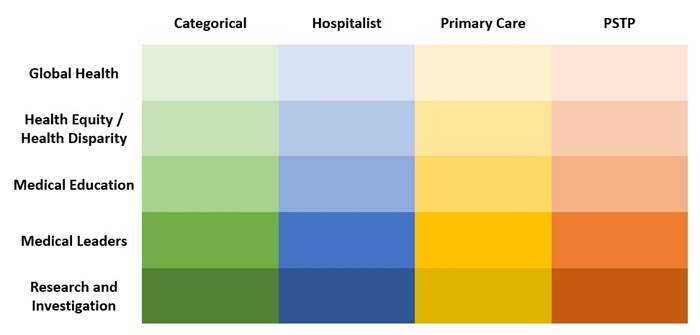
Each training track (Categorical, Primary Care, Hospitalist, and PSTP) has its own curricular content. At the beginning of the second year, every resident also selects one of five pathways (Global Health, Health Equity & Policy, Medical Education, Medical Leaders, and Research & Investigation). With 4 different training tracks and 5 different career pathways, there are 20 formal curricular combinations available to our residents. Right now, there are residents who inhabit each of these educational homes and with whom you will get to work during your training.
The matrix below demonstrates how residents are able to individualize their residency training:
Take a Deep Dive into our Curricular Offerings:
In addition to selecting a track and pathway, every resident will engage with several curricular experiences across their residency training to enhance their educational growth. These offerings include:
Wednesday Education Session (WES)
Residents attend an educational half day, WES (Wednesday Education Session), during their non-call blocks throughout residency for a total of 24 sessions per year. Residents are excused from clinical responsibilities in order to focus on the educational opportunities at hand. We have steadily moved away from traditional lecture-based content to small interactive group and case-based learning led by faculty and chief medical residents. We also incorporate the NEJM resident 360/knowledge+ platform for independent learning and quizzes to reinforce concepts covered during WES. The curriculum covers core clinical knowledge, foundational skills including ECG, CXR, procedure simulation, clinical reasoning, and point of care ultrasound, and other key topics including health inequities, systems of care, career development, and physician wellness. Finally, residents receive the foundational content for each pathway during their intern year and then elect to continue in one pathway during their second and third years.
Noon Conference
Noon conference occurs Monday-Friday at our inpatient clinical sites (University Hospital, Denver Health, and the VA). Food is provided and ancillary staff are reminded this is a protected, required time for resident education. Noon conference is structured like many programs might hold Morning Report with a diverse array of conference formats often focused on cases currently at the hospital. The chief residents run each noon conference with occasional expert guest speakers. The chief residents aim to provide a balanced review of Internal Medicine specialties, health systems science, and evidence-based medicine, while incorporating important themes in humanism, diversity, and equity. On Wednesdays throughout the year, this hour is used to watch world experts discuss the newest research through the University of Colorado Department of Internal Medicine Grand Rounds series.
Point of Care Ultrasound Curriculum
The University of Colorado Internal Medicine Residency Program Point of Care Ultrasound (POCUS) Curriculum is a longitudinal learning experience that aims for the residents to learn fundamental POCUS knowledge and apply basic POCUS skills to incorporate POCUS into clinical care safely. The curriculum is integrated into and taught longitudinally during the Wednesday Education Sessions during the resident’s ambulatory block. Expert faculty members deliver POCUS didactics.
| Curricular Structure | Topics Covered |
|
|
Rapid Access Clinic
The Rapid Access Clinic (RAC) is a quazi-urgent care clinic at the VA. All first- and third-year residents spend one block on RAC. It offers our residents a rich experience in problem-focused outpatient care with a structured curriculum including simulation-based outpatient procedure training, ambulatory point-of-care ultrasound, transitions of care, and management of decompensated chronic diseases (e.g., heart failure, liver failure, COPD, and diabetes).
Comprehensive Procedural Curriculum
We have developed a full spectrum approach to procedure training that includes procedural checklists standardized across all three hospital sites, locally developed procedural videos, rotation-paired simulation training during protected educational time, and real-time digital assessments to provide specific and actionable feedback.
New England Journal of Medicine Knowledge+
Every resident has a NEJM resident 360 account, giving them access to rotation prep (Rotation Prep | NEJM Resident 360) with topic overviews, links to landmark clinical trials and review articles, practice guidelines, and additional resources including interactive case modules and videos for every core Internal Medicine topic. They also have a Knowledge+ account (NEJM Knowledge+ - Home), with 6000+ ABIM board style questions.
Clinic Didactics
During each of the three continuity clinic months, residents from all tracks have one-half day a week of protected didactic time. Didactics consist of a core primary care curriculum (eg. hypertension, diabetes, women's health), various advanced primary care topics (eg. medication-assisted treatment, sports medicine), and outpatient subspecialty topics including both medicine subspecialties and others related to primary care (eg. dermatology). Our didactics are led by a mix of chief residents, core primary care faculty, subspecialty guests, and residents who are interested in medical education. We integrate education on social determinants of health, QI, and practical clinic skills like agenda setting and EMR efficiency into each week.
Thursday Education Session (TES)
Interns in the Primary Care track attend weekly dedicated curricular sessions for two months out of their first year (8 Thursday mornings across July and March). These sessions are specific to helping them better understand their roles as primary care physicians, particularly with a focus on social determinants of health and community engagement in the first year. After intern year, upper-level residents will engage in WES during their outpatient and elective months where 6 of these sessions (12 total sessions as an upper level) are dedicated to the Primary Care track curriculum. You can learn more about the TES Curriculum on the Primary Care Track webpage.