Our Vision
To create an integrated research ecosystem for our research teams to make transformative discoveries that improve lives.
Our Research
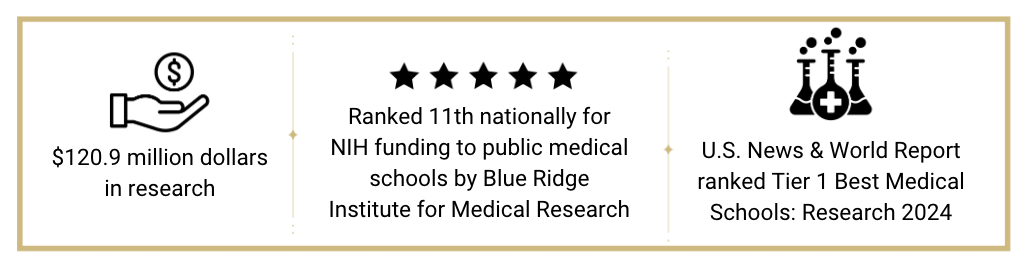
The Department of Medicine is a national leader in biomedical research, consistently ranking in the top 25 for NIH funding and doubling the growth of NIH support over the past five years. Our faculty are renowned for their innovation and dedication to advancing human health, making significant contributions to biomedical knowledge and transforming healthcare delivery.
By the Numbers
Research Opportunities and Resources
DOM Post-Award Services
- Financial, transactional and analytical support related to post-award grant management for DOM divisions. For access to this support or to ask specific post-award questions, please email the Research Office at DOMResearch@cuanschutz.edu.
Library of Example Grant Components
- Thanks to our incredible DOM faculty members, we have compiled a library of example grant components, including facilities and resources, vertebrate animals, human subjects, data management and sharing plans, letters of support, and more! These examples can only be accessed using your university login. Please contact us for any further questions or support.
CU Anschutz Research Cores
- Operational core labs provide efficient cost-effective services for your research. Find services and contact information for 53 core facilities here.
Looking for a Researcher? Find them here.
Contact Us
Research Investment in the Scientific Enterprise (RISE)
- RISE provides financial support for DOM faculty who obtain extramural funding at the NIH P-, U-, or R01-levels. All DOM faculty are eligible for these funds, based on the direct costs of qualifying extramural award/s.
- RISE Policy determines eligibility and level of funding. Upload your NIH Notice of Grant Award (NOGA) or equivalent to receive RISE.
SOM Bridge Funding Match
- For one year, DOM will match funds provided through the SOM bridge funding program for eligible DOM faculty. If you received SOM Bridge Funding after January 1, 2024, upload your letter from the SIRC here to be eligible.
DOM Financial Contributions and Letters of Support (LOS) for Large Grants and Core Resources
- Read the policy about requests for financial contributions and letters of support from the DOM here.
- Online requests are evaluated monthly and must be received at least three weeks before the application due date.
Collaborative Opportunities for Advancing Research and Translational Efforts in the Department of Medicine (COLLABORATE DOM) Program
COLLABORATE supports new research collaborations between DOM Divisions and CU Anschutz departments and schools. It aims to advance research and discovery by promoting collaboration among basic, translational, and clinical researchers. These awards support interdisciplinary research through two phases:
1. Team Formation 2. Pilot Awards
Team formation awards are $3,000 over 6 months to develop a proposal detailing team members, roles, specific aims, preliminary data, and a timeline for submitting an MPI NIH R01 grant, SOM ASPIRE application, or equivalent.
Pilot awards provide $40,000 over 12 months for preliminary data supporting MPI applications. Up to three awards are funded annually. Awardees must: 1. Submit a co-authored manuscript to a peer-reviewed journal within 12 months. 2. Submit an MPI R01 or equivalent within 18 months, or a SOM ASPIRE application within 12 months.
Online applications for both the team formation and pilot awards are accepted yearly in May. The online submission portal opens yearly in mid-April.
Reach Achievement Highlights (REACH)
- Monthly REACH forums include 2-4 brief presentations in under an hour, describing the challenges and triumphs of research. Real, relatable experiences of your peers that may inspire you in your own research journey. Presentations 3:30-4:30 PM, with no questions at the podium - presenters and DOM leaders will answer all of your questions during the networking over nibbles hour, 4:30-5:30 PM, immediately following the presentations.
- Topics showcase work across all divisions and the whole research spectrum, T0-T4.
- November 19, 2024 - Dynamic Duos: The power of the mentor-mentee relationship to accelerate career success
- January 21, 2025 - Research Town Hall with Research Leadership
Collaborative Opportunities for Advancing Research and Translational Efforts in the Department of Medicine (COLLABORATE DOM) Program
COLLABORATE supports new research collaborations between DOM Divisions and CU Anschutz departments and schools. It aims to advance research and discovery by promoting collaboration among basic, translational, and clinical researchers. These awards support interdisciplinary research through two phases:
1. Team Formation 2. Pilot Awards
Team formation awards are $3,000 over 6 months to develop a proposal detailing team members, roles, specific aims, preliminary data, and a timeline for submitting an MPI NIH R01 grant, SOM ASPIRE application, or equivalent.
Pilot awards provide $40,000 over 12 months for preliminary data supporting MPI applications. Up to three awards are funded annually. Awardees must: 1. Submit a co-authored manuscript to a peer-reviewed journal within 12 months. 2. Submit an MPI R01 or equivalent within 18 months, or a SOM ASPIRE application within 12 months.
Online applications for both the team formation and pilot awards are accepted yearly in May. The online submission portal opens yearly in mid-April.
Research Day
- Research Day is an annual showcase of the Department of Medicine's diverse and exciting achievements in basic, translational, clinical and outcomes research. It is designed to encourage lively discussions and multidisciplinary collaborations across fields of medicine.
- Click here to learn more about Research Day.
9-week Grant Writing Workshop for First to Second R01 Applications
- Faculty grant proposal development workshop program to provide dedicated writing time, develop proposals, provide peer support and provide detailed feedback from grant writing experts and senior faculty in the Department of Medicine.
- Intensive 9-week program for faculty who are actively developing NIH R01 or VA/DOD R01-equivalent proposals for submission.
- Topics include specific components of the proposal: the Specific Aims page, Significance, Innovation, Approach, Introduction (for resubmissions), and the Biosketch.
- The workshops are led by Jennifer Kemp, PhD, Director of DOM Research Office, with expert input from senior DOM faculty and leadership. There will be an emphasis on strong grantsmanship and clear communication.
- Spring 2025 workshops begin March 12, 2025.
- Registration opens January 2025.
Research Grant Proposal Development Seminars
Join us to learn more about important aspects of grant writing, and to develop strong proposals for NIH and other funding agencies.
Topics include:
- Specific AIMS: how to write a compelling aims page by telling the story of your science.
- December 10, 2024 from 11 AM-12 PM in AHSB P12-2201
- The Research Plan: Conveying significance and innovation and "selling reviewers."
- January 14, 2025 from 1-2 PM in AHSB P12-1204
- Resubmissions: Writing a responsive revision to address reviewer concerns and improve your proposal.
- February 12, 2025 from 1-2 PM in AHSB P12-1204
- Other Critical Grant Elements: Biosketches, letters of support, and other small but important sections to tell your story and highlight your strengths.
- March 11, 2025 from 10-11 AM at AHSB P12-1204
- NIH Review Process: What actually happens during study section meetings? Q&A with a panel of NIH Study Section reviewers.
- May 13, 2025 from 1-2 PM at AHSB P12-2201
Format is a series of five (5) stand-alone seminars and participants may attend as few or as many as they choose. Open to all DOM researchers with no application or preregistration required. Seminars are led by Jennifer Kemp, PhD, Director of the DOM Research Office.
Specific Aims Page Workshop
- Two-session grant writing workshop focused on developing outstanding Specific AIMS pages for applying to external grant funding agencies such as the NIH.
Session 1: February 25, 2025 from 9:30-11 AM in AHSB P12-2200/2201
Didactic presentation, including best practices for writing a compelling specific aims page, followed by discussion time (1-1.5 hours). Participants will learn:
- How to grab the reviewers' attention and stand out from the pack.
- How to tell your story.
- Advice on how to structure this critical 1 page overview of your proposal.
- Critical elements to include on the aims page.
- Common mistakes to avoid.
Session 2: March 25, 2025 from 9:30-11:30 AM in AHSB P12-2200
The second session will be an interactive workshop format, in which we will critique each other's specific aims pages and work to improve them (3-4 hours).
- This 2-session workshop is open to all DOM faculty. Space is limited, and those working on their first or second R01 or R01-equivalent proposal will be prioritized for admission.
- The specific aims development workshop is limited to 10-12 participants and is led by Jennifer Kemp, PhD, Director of the DOM Research Office.
Grant Pre- and Post-Award Training
- We will provide ongoing support and training sessions for division administrators regarding pre and post-award processes via zoom on the first Thursday of every month. Please email DOMResearch@cuanschutz.edu to be added to the meeting invites.
- We hold bi-monthly research meetings for division administrators and staff to stay updated on campus processes, policy changes, federal sponsor updates, and best practices. Topics include financial management training, pre- and post-award support, and campus resources. For access, email the Research Office at DOMResearch@ucdenver.edu.
Professional Development for CU Research Professionals:
- The Clinical Research Workforce Development initiative through the Office of the Vice Chancellor for Research supports the connectivity, training and career development of clinical research professionals at CU Anschutz.
Faculty Development:
- For events, resources, and information regarding mentoring, promotion, wellbeing, and DEI, please visit the DOM Faculty and Staff Development.
Questions?
Contact: DOMResearch@cuanschutz.edu