Contact UCHealth
Thyroid Cancer
Clinical Trials
Make a Gift
What Is Thyroid Cancer?
The thyroid gland is at the base of the throat just above the collarbone. It is thumb-size and shaped like a butterfly, with a lobe on the right and left sides of the trachea. As part of the endocrine system, it produces hormones that help regulate blood pressure, metabolism, heart rate, weight, and body temperature.
Thyroid cancer is a type of cancer that begins in the thyroid gland and can spread to nearby tissues and other areas of the body.
According to the American Cancer Society, approximately 44,020 new cases of thyroid cancer are diagnosed in the United States each year, with an estimated 2,170 deaths.
In Colorado, there are an estimated 710 new cases diagnosed annually.
Thyroid Cancer Prognosis and Survival Rates
Thyroid cancer five-year relative survival rates vary depending on the type of thyroid cancer, how far the cancer has spread, age and overall health, how well it responds to treatment, and other factors.
However, the two most common types of thyroid cancer, papillary and follicular, have encouraging five-year relative survival rates. For papillary thyroid cancer, the rate is near 100%, and is 98% for follicular.
The rates are lower in instances in which the cancer spreads to distant parts of the body, such as the bones, but still are 74% for papillary and 67% for follicular.
Why Come to CU Anschutz Cancer Center for Thyroid Cancer
The CU Anschutz Cancer Center is the only National Cancer Institute Designated Comprehensive Cancer Center in Colorado and one of only four in the Rocky Mountain region.
The Cancer Center is home to a variety of specialists with expertise in treated thyroid cancer. The CU Endocrinology Thyroid Program, with a nationally recognized team specializing in the evaluation and management of thyroid cancer, that provides innovative, personalized care – from diagnosis through treatment of advanced disease.
Experts in the Endocrine Thyroid Program use on-site advanced technology to offer cutting-edge evaluation, and are part of a multi-disciplinary approach to providing comprehensive, state-of-the-art treatment options. The CU Anschutz Cancer Center hosts several multi-disciplinary clinics for patients with thyroid cancer, including joint surgical and endocrinology clinics for earlier stage disease, and combined medical oncology and endocrinology clinics for patients with advanced cancers.
Contact the Thyroid Multidisciplinary Clinic at 720-848-3299.
The program also features UCH Thrive, a clinical program for patients with thyroid cancer who are stable or in remission. It emphasizes overall health and well-being, shifting the focus from active cancer treatment to monitoring disease stability.
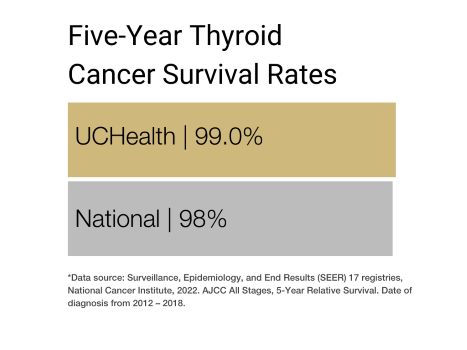
Our clinical partnership with UCHealth has helped lead to thyroid cancer survival rates higher than the Colorado average for all stages of thyroid cancer.
For more information on pediatric thyroid cancer care at our clinical partner, and to learn more about the care options and endocrinology, visit the Pediatric Thyroid Cancer and Nodule Program at Children’s Hospital Colorado.
There are two main types of cells in the thyroid gland:
- C cells, which make a hormone called calcitonin that helps control how bodies use calcium
- Follicular cells, which make thyroid hormones from iodine in the blood and help regulate metabolism
This distinction is important because different cancers can develop in each cell type. That impacts how serious the cancer is and how it’s treated.
Types of Thyroid Cancer
The main types of thyroid cancer are papillary, follicular, medullary, and anaplastic.
- Papillary thyroid cancer is the most common, accounting for between 70 and 80 percent of all thyroid cancers in the United States. This type of thyroid cancer generally grows slowly and often in just one lobe of the thyroid gland. Despite its slow growth, it can spread to lymph nodes in the neck. However, even if papillary thyroid cancer spreads to the lymph nodes, it often can be successfully treated and is not often fatal.
- Follicular thyroid cancer represents 10 to 15 percent of all thyroid cancer in the United States. It is more common in areas in which people don’t get enough iodine in their diets. Follicular thyroid cancer generally doesn’t spread to the lymph nodes, but can spread to other parts of the body. While five-year relative survival rates aren’t quite as high as they are for papillary thyroid cancer, the outlook is still very good in most cases.
- Medullary thyroid cancer represents about 4 percent of all thyroid cancers and develops from the C cells in the thyroid gland. It is able to spread to lymph nodes and other parts of the body, and can be difficult to detect and treat.
- Anaplastic thyroid cancer is quite rare and represents less than 2 percent of all thyroid cancer. It can spread quickly through the neck and other parts of the body and can be very difficult to treat.
Risk Factors for Thyroid Cancer
As with most types of cancer, scientists have identified several risk factors that make a person more likely to develop thyroid cancer. Some of these factors can’t be changed and some can. Among the risk factors that can’t be changed are:
- Age and gender: Women are about three times more likely to develop thyroid cancer than men. And while it can occur at any age, women are most often in their 40s and 50s when they receive a thyroid cancer diagnosis, while men are in their 60s and 70s.
- Hereditary conditions: While most people who develop thyroid cancer do not have a family history of the disease or an inherited condition, several conditions have been linked to the disease. These include inheriting mutations in the RET gene, such as MEN2, as well as a family history of other thyroid cancers, familial adenomatous polyposis (FAP), Cowden disease, Carney complex type I, and familial non-medullary thyroid carcinoma.
- Family history: An increased risk for thyroid cancer can be linked to first-degree relatives with thyroid cancer.
Among the risk factors for thyroid cancer that may be changed are:
- Exposure to radiation: This may include certain medical treatments and fallout from nuclear weapons or power plant accidents. An increased risk for thyroid cancer may be traced to head or neck radiation treatments received in childhood.
- Being overweight or obese: The International Agency for Research on Cancer has found that the risk of developing thyroid cancer increases as body mass index (BMI) increases.
- Low iodine in the diet: Follicular thyroid cancer is more common in parts of the world where diets are low in iodine. People in the United States generally get enough iodine in their diets because it is added to table salt and other foods.
Symptoms of Thyroid Cancer
A particular concern with thyroid cancer is that it often doesn’t cause early symptoms or signs. Sometimes it may be found during a routine physical exam, while other time signs and symptoms don’t occur until the tumor has grown. Consult your doctor if you experience:
- Pain when swallowing.
- Trouble breathing.
- Trouble swallowing.
- A lump in your neck that you can feel through the skin.
- Hoarseness or other changes in your voice.
- Swollen lymph nodes in your neck.
If you have any of these symptoms, speak with your doctor right away. Many of these signs and symptoms also can indicate non-cancerous conditions, but it’s important to see your doctor so their cause can be diagnoses and treated, if necessary.
Diagnosing Thyroid Cancer
Generally, one of the first steps your physician will take is to get a complete medical history. This may include questions about your family history, risk factors, symptoms, and other health concerns or problems. If someone in your family has had thyroid cancer, you may be at increased risk.
Your physician also will complete a physical exam to get more information about the signs and symptoms of thyroid cancer you may be experiencing, as well as any other health problems. The exam may include special attention to the size and firmness of your thyroid and the lymph nodes in your neck.
This may be followed by different tests, including:
Imaging tests
- Ultrasound: This test uses sound waves to determine whether a thyroid nodule is solid or filled with fluid – solid nodules are more likely to be cancerous. It also can determine the size and number of thyroid nodules, as well as whether the nearby lymph nodes are enlarged.
- X-ray: If you have received a thyroid cancer diagnosis, your doctor may order a chest x-ray to determine whether cancer has spread to your lungs.
- CT scan: This may be used to determine the size and location of thyroid cancers and whether they have spread to other organs or areas nearby.
- MRI: An MRI scan can locate cancer in the thyroid and provide thorough images of the thyroid gland.
- PET scan: This diagnostic tool may be used if the thyroid cancer doesn’t absorb radioactive iodine during a radioiodine scan. It may help determine whether the cancer has spread.
Biopsy
A biopsy is used to make the actual thyroid cancer diagnosis. It is one of the most common ways to determine whether a nodule or lump on the thyroid gland is cancerous, and usually is done via fine-needle aspiration (FNA).
Your doctor may inject local anesthesia into the skin over the nodule before performing the biopsy, but often this isn’t necessary. Then, your doctor will use a thin, hollow needle to take some cells and fluid from the nodule. These are then sent to a lab to determine whether they are cancerous or benign. Biopsies generally are performed on nodules that are big enough to feel through the skin.
Lab tests of biopsy samples
Sometimes doctors will order molecular tests on cell and fluid samples taken during the biopsy. These may be to look for changes in certain genes related to thyroid cancer, or to see if existing cancer cells have changes in certain genes.
Blood tests
Your doctor won’t use blood tests to find thyroid cancer, but may use them to determine whether your thyroid gland is working like it should be. The results of blood tests may help your doctor determine whether other tests are needed.
Stages of Thyroid Cancer
After you have received a thyroid cancer diagnosis, your doctor will next work to determine the type of thyroid cancer and whether or how far the cancer has spread, a process called staging. The different stages help describe not only how much the cancer has spread and how much of it there is in your body, but also help determine the best way to treat it.
Staging is generally determined by the size of the tumor, whether it has spread to nearby lymph nodes and whether it has spread to distant organs.
Staging for thyroid cancer is determined by the type of thyroid cancer and the age of the patient
For patients younger than 55 with papillary or follicular thyroid cancer:
- Stage I: The tumor may be any size and may have spread to nearby lymph nodes and tissue, but not other parts of the body
- Stage II: The tumor may be any size, cancer may have spread to nearby lymph nodes and tissue, and also has spready to other parts of the body such as bones or lungs.
For patients 55 and older with papillary or follicular thyroid cancer:
- Stage I: Cancer is isolated to the thyroid and the tumor is smaller than 4 centimeters.
- Stage II: Cancer is found in the thyroid, the tumor is smaller than 4 centimeters, and cancer has spread to nearby lymph nodes; or cancer is found in the thyroid, the tumor is larger than 4 centimeters, and the cancer may have spread to nearby lymph nodes; or the tumor is any size and the cancer has spread from the thyroid gland to nearby neck muscles, and also may have spread to nearby lymph nodes.battle that
- Stage III: The tumor is any size, cancer has spread from the thyroid to the traches, the larynx, the esophagus, soft tissue under the skin, or the recurrent laryngeal nerve, and cancer may have spread to lymph nodes.
- Stage IVA: The tumor is any size, the cancer has spread to tissue in front of the spine or has surrounded the blood vessels in the area between the lungs or around the carotid artery, and may have spread to lymph nodes.
- Stage IVB: The tumor is any size, cancer has spread to other parts of the body, such as the bones or lungs, and may have spread to lymph nodes.
For patients of all ages with anaplastic thyroid cancer, which grows quickly and is considered a stage IV thyroid cancer:
- Stage IVA: Cancer is found only in the thyroid and the tumor may be any size.
- Stave IVB: Cancer is found in the thyroid, the tumor may be any size and the cancer has spread to nearby lymph nodes; or the tumor is any size, cancer has spread from the thyroid to nearby neck muscles, and may have spread to nearby lymph nodes; or the tumor is any size, the cancer has spread from the thyroid to soft tissue under the skin, the trachea, the larynx, the esophagus, tissue in front of the spine, or the recurrent laryngeal nerve, or has surrounded the carotid artery or the blood vessels in the area between the lungs, and the cancer may have spread to lymph nodes.
- Stave IVC: The tumor is any size, the cancer has spread to other the parts of the body, and may have spread to lymph nodes.
For patients of all ages with medullary thyroid cancer:
- Stage I: The cancer is smaller than 2 cm and confined to the thyroid, and has not spread to lymph nodes or distant sites
- Stage II: The cancer is larger than 2 cm but no more than 4 cm across and confined to the thyroid; or it is larger than 4 cm and confined to the thyroid or any size and growing outside the thyroid but doesn’t involve nearby structures. It has not spread to nearby lymph nodes or to distant sites.
- Stage III: The cancer is any size and may be growing outside the thyroid but does not involve nearby structures, or it has spread to lymph nodes in the neck but not other lymph nodes or distant sites.
- Stage IVA: The cancer is any size and may be growing outside the thyroid but does not involve nearby structures, or it has spread to certain lymph nodes in the neck but not to distant sites; or it is any size and has grown beyond the thyroid to nearby tissues in the neck, and may or may not have spread to nearby lymph nodes.
- Stage IVB: The cancer is any size and has grown into nearby blood vessels or back to the spine, and may or may not have spread to nearby lymph nodes but not distant sites.
- Stage IVC: the cancer is any size and may have grown into nearby structures. It alsy may or may not have spread to nearby lymph nodes and has spread to distant sites such as the brain, liver, lungs, or bones.
Treatments for Thyroid Cancer
Currently there are six standard treatments for thyroid cancer, and the course of treatment that will be most effective may be determined by type and stage of thyroid cancer, your general health, and other factors.
If it hasn’t spread to distant parts of the body, thyroid cancer generally responds very well to treatment. If the cancer can’t be completely eradicated, a goal of treatment may be to destroy or remove as much cancer as possible and keep it from growing, spreading, or returning.
Surgery for Thyroid Cancer
Surgery is the most common treatment for thyroid cancer. This could include:
- Lobectomy, during which the lobe of the thyroid gland in which the cancer was found is removed
- Near-total thyroidectomy, in which all but a very small part of the thyroid gland is removed.
- Total thyroidectomy, which is removal of the whole thyroid gland
Radiation Therapy for Thyroid Cancer
Radiation therapy is a cancer treatment in which high-energy x-rays or other radiation are used to kill cancer cells or keep them from growing. There are two different kinds of radiation that can be used to treat thyroid cancer. Radioactive iodine is given by mouth to treat intermediate or high risk papillary or follicular thyroid cancers after surgery. . External beam uses x-rays to treat cancers.
It may be given after surgery to kill any cancer cells that weren’t removed during surgery.
Chemotherapy for Thyroid Cancer
Chemotherapy is a cancer treatment that kills cancer cells, or stops them from dividing, with drugs that enter the body either through the bloodstream or by being placed directly into an organ, body cavity, or the cerebrospinal fluid. Chemotherapy is rare used to treat thyroid cancer.
Thyroid Hormone Therapy
Thyroid hormone therapy is a cancer treatment that either removes certain hormones or blocks their usual actions and stops cancer cells from growing. In this therapy, drugs are used to prevent the body from making thyroid-stimulating hormone, which helps lower the risk of the thyroid cancer returning or continuing to grow.
Targeted Therapy for Thyroid Cancer
Targeted therapy is a treatment that uses drugs or other substances to identify and attack cancer cells. Targeted therapy is generally less harmful to normal cells than chemotherapy and radiation. There are two types of targeted therapy:
- Multikinase inhibitors, which blocks the signals needed for tumors to grow. Examples include Lenvatinib and cabozantinib.
- Mutation-specific kinase inhibitors, which blocks proteins needed for cell growth. Examples include pralsetinib, dabrafenib, and Larotrectinib.
Active Surveillance for Thyroid Cancer
Watchful waiting means closely monitoring a patient’s signs and symptoms without treatment, and reassessing if those signs and symptoms change.
Clinical Trials
At any given time, the University of Colorado Cancer Center offers a wide variety of clinical trials for patients with thyroid cancer.
Latest in Thyroid Cancer from the Cancer Center
Loading items....
Information reviewed by Daniel Bowles, MD, in February 2022.