Contact UCHealth
Multiple Myeloma
Clinical Trials
Make a Gift
What Is Multiple Myeloma?
Multiple myeloma is a hematologic cancer that begins in plasma cells, a type of white blood cell that makes antibodies to protect against infection.
Normal plasma cells are an important part of the immune system and are found in the bone marrow. In multiple myeloma, cancerous plasma cells, called myeloma cells, crowd out normal plasma cells, healthy red blood cells, white blood cells, and platelets. Instead of normal antibodies, these cancerous plasma cells produce too many identical copies of an antibody called monoclonal protein, or M-protein. M-protein can cause complications such as bone tumors, kidney damage, low blood counts, and immune compromise.
According to the American Cancer Society, approximately 34,920 new cases of multiple myeloma are diagnosed in the United States each year, with an estimated 12,410 deaths. In Colorado, there are an estimated 490 new cases diagnosed annually and 200 deaths.
Multiple Myeloma Prognosis and Survival Rates
The American Cancer Society tracks five-year survival rates for multiple myeloma using the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) database. This data groups cancers into localized, regional, and distant stages. At the localized stage, only one tumor, called a solitary plasmacytoma, is growing in or outside the bone. At the distant stage, multiple tumors are found, leading to the diagnosis of multiple myeloma. The staging of multiple myeloma does not depend on the number or location of tumors like solid tumors, but rather on genetic factors in the tumors and other blood markers that signify tumor aggressiveness.
Currently, with optimal treatment including autologous stem cell transplant and lenalidomide maintenance, the average survival is more than 10 years.
Why Come to CU Cancer Center for Multiple Myeloma
The CU Cancer Center is the only National Cancer Institute-Designated Comprehensive Cancer Center in Colorado and one of only four in the Rocky Mountain region.
CU Cancer Center researchers and physicians are world leaders in blood cancer breakthroughs and the best in the Rocky Mountain region for stem cell transplant outcomes.
Patients also may be eligible for ongoing clinical trials, which provide additional options along with transitional multiple myeloma treatments. CU Cancer Center physicians are leaders in stem cell and bone marrow transplants for multiple myeloma. They also are on the cutting edge of research and have made exciting breakthroughs in developing immunotherapies for multiple myeloma.
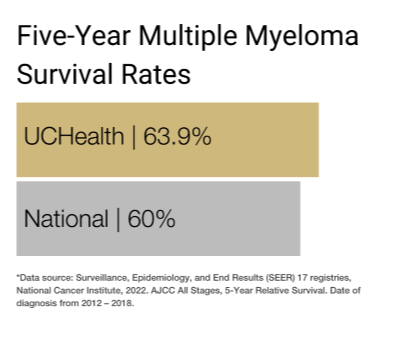
Our clinical partnership with UCHealth has produced survival rates higher than the state average for all stages of multiple myeloma.
Risk Factors for Multiple Myeloma
In the past few decades, researchers have made significant progress in understanding how certain changes to DNA can cause plasma cells to become cancerous. In about half of people with myeloma, part of one chromosome switches with part of another chromosome in myeloma cells, a form of mutation that is called a translocation.
Types of Multiple Myeloma
While there is a spectrum of plasma cell disorders, only when plasma cells grow uncontrollably and cause symptoms is the condition considered active multiple myeloma. The plasma cell disorders that may not meet the criteria to be considered active multiple myeloma include:
- Monoclonal gammopathy of undetermined significance (MGUS), which occurs when clonal plasma cells make up less than 10% of cells in the bone marrow. MGUS is generally considered a precancerous condition and has no symptoms. There is a low risk of advancing to active disease for most patients with MGUS.
- Smoldering multiple myeloma (SMM) is also considered precancerous, but the clonal plasma cells make up greater than 10% of the bone marrow. SMM is also asymptomatic. Patients with SMM are more likely to progress to active myeloma than patients with MGUS.
- Solitary plasmacytoma is a single tumor that develops in a bone or other tissue but has not spread to other parts of the body. This condition is typically curable by surgery or radiation treatment.
- Light chain amyloidosis occurs when clonal plasma cells produce an antibody protein that tends to deposit in patient tissues, causing a variety of potential complications.
Active multiple myeloma is generally diagnosed with higher levels of plasma cells in the bone marrow and symptoms that comprise the CRAB criteria: calcium elevation, renal dysfunction, anemia, and bone disease, such as bone lesions.
Risk Factors for Multiple Myeloma
There are several risk factors that may affect a person’s chance of being diagnosed with multiple myeloma, though it is important to remember that risk factors don’t tell the entire story of cancer.
For multiple myeloma, risk factors can include:
- Age: The risk of being diagnosed with multiple myeloma increases with age, and fewer than 1% of cases are diagnosed in those 35 or younger. The majority of cases are diagnosed in those age 65 or older.
- Gender: Males have a slightly greater chance of developing multiple myeloma than females.
- Race: Multiple myeloma is found almost twice as often in people who are Black than in people who are White, and the reasons for this are unknown.
- Weight: People who are overweight or obese are at increased risk for developing multiple myeloma.
- Family history: There is evidence that people who have siblings or parents diagnosed with multiple myeloma are slightly more likely to be diagnosed than people without that family history. However, the vast majority of patients with multiple myeloma have no family history of the disease.
Symptoms of Multiple Myeloma
Multiple myeloma is a challenging cancer because it can be difficult to diagnose. People frequently do not experience symptoms until multiple myeloma has reached a high burden of disease. It sometimes can be found early if results from a blood test show abnormally high amounts of M-protein in the blood. One of the most common first symptoms people experience is bone pain, often in the back, hips, chest, or skull.
Other symptoms include:
- Bone weakness or fracture.
- High levels of calcium in the blood, which can cause extreme thirst, frequent urination, severe constipation, abdominal pain, loss of appetite, drowsiness, or confusion.
- Infections.
- Impaired kidney function or kidney failure.
- Low blood cell count.
- Mental fogginess.
- Excessive thirst.
- Loss of appetite.
- Constipation.
- Anemia.
- Fatigue or low energy.
Diagnosing Multiple Myeloma
If a person has multiple myeloma symptoms, there are several ways to determine whether they have the disease. These include:
Lab tests
- A complete blood count: This test measures how many red cells, white cells, and platelets are in the blood. If there are myeloma cells in the bone marrow, the red, white, and platelet counts may be low.
- Urine test: Common urine tests called urine protein electrophoresis (UPEP) and urine immunofixation may be used to find M-protein that gets filtered through the kidneys.
- Blood chemistry test: This test measures levels of calcium, creatinine, albumin, or other electrolytes. High levels of creatinine may show that the kidneys are not functioning well, which is common in multiple myeloma. High calcium levels are common in those with advanced multiple myeloma, as are low levels of albumin, a blood protein.
- Quantitative immunoglobulin test: This test measures different types of antibodies, or immunoglobulins, in the blood. With multiple myeloma, one type of immunoglobulin may be high while another is low.
- The most specific blood tests to diagnose multiple myeloma are the serum protein electrophoresis (SPEP) and serum free light chain blood tests.
Biopsy
- Bone marrow aspiration and biopsy: In this procedure, the back of the iliac bone in the pelvis is numbed with local anesthetic, and a needle is inserted into the bone to remove a small amount of liquid marrow contents (aspiration) or a solid-tissue piece of bone marrow (biopsy).
Imaging tests
- Bone x-ray: An x-ray can help locate areas of bone that have been damaged or destroyed by myeloma cells.
- Computed tomography (CT) scan: A CT scan uses x-rays directed from multiple angles and combines them with a computer to draw detailed pictures of bones or organs. A CT scan can help determine whether myeloma cells have damaged bones.
- Magnetic resonance imaging (MRI) scan: Using strong magnets and radio waves, an MRI can create detailed images of soft tissue, bone, and bone marrow.
- Positron emission tomography (PET) scan: During this scan, a type of radioactive sugar is injected into a vein so it can travel through the body. Cancer cells absorb high amounts of this sugar, and a special camera is used to see the areas of the body in which the sugar is collected.
Multiple myeloma is often diagnosed by considering a patient’s symptoms, conducting tests and analyzing the results, and the physician’s physical examination of the patient. A multiple myeloma diagnosis requires over-proliferation of monoclonal plasma cells found through a biopsy and at least one of the following:
- High blood calcium level.
- Poor kidney function.
- Low red blood cell counts (anemia).
- Bone tumors found in imaging studies (CT, MRI, PET scan).
- Increase in one type of light chain in the blood so that one type is 100 times more common than the other.
- 60% or more myeloma cells in the bone marrow.
Stages of Multiple Myeloma
Physicians use the Revised International Staging System (R-ISS) to determine a patient’s prognosis from multiple myeloma. The R-ISS looks at four factors:
- The amount of albumin in the blood. Albumin is a protein found in blood plasma and can be decreased in higher risk disease.
- The amount of beta-2-microglobulin in the blood. Beta-2-microglobulin is a small protein normally found in the blood and can be highly elevated in some high-risk disease.
- The amount of LDH in the blood. LDH is an enzyme found in many different tissues, and elevated levels can occur in some cases of high-risk disease.
- The specific gene abnormalities (cytogenetics) of the cancer.
In RISS stage group I, factors are:
- Albumin level is 3.5 (g/dL) or greater.
- Serum beta-2 microglobulin is less than 3.5 (mg/L).
- LDH levels are normal.
- Cytogenetics are considered “not high risk”.
In RISS stage group II, factors are not stage I or stage III
In RISS stage group III, the most aggressive factors are:
- Serum beta-2 microglobulin is 5.5 (mg/L) or greater.
- Cytogenetics are considered “high-risk”.
- LDH levels are high.
Physicians may also consider factors such as kidney function, age, and overall health when staging multiple myeloma.
Treatments for Multiple Myeloma
Multiple myeloma is typically treated with systemic therapy, which affects the whole body. In some cases, local treatments may be added to help manage specific symptoms or complications.
Systemic treatments are drugs given orally, with shots beneath the skin, or directly into the bloodstream. They may reach cancer cells found anywhere in the body and include
Drug therapy for multiple myeloma
There are many different drugs that are very effective to treat multiple myeloma, including:
Proteasome inhibitors, which stop enzyme complexes (proteasomes) in cells from breaking down the byproducts of M-protein production. They effectively cause the myeloma cells to die from their own internal garbage.
Immunomodulatory drugs, which lead to the degradation of key proteins that support the survival of myeloma cells.
Monoclonal antibodies, which are proteins made by the body’s immune system to fight infections. Synthetic monoclonal antibodies have been designed to attack specific targets on myeloma cells.
Steroids, which in high doses have the ability to kill multiple myeloma cells.
Conventional chemotherapies may also sometimes be used.
It is common for several drug therapies to be used in combination for treating multiple myeloma, though each person’s course of treatment will be determined based on their individual case.
Stem cell transplant for multiple myeloma
Most patients undergo an autologous stem cell transplant, one in which the stem cells are mobilized from their own bone marrow and taken from their blood. The patient receives high-dose chemotherapy to kill the blood cells in the bone marrow. Then the patient receives new, healthy stem cells that form blood. It is rare for an allogeneic stem cell transplant, in which stem cells are transferred from a donor, to be used in multiple myeloma.
CAR T-cell therapy for multiple myeloma
Chimeric antigen receptor (CAR) T-cell therapy is a type of cancer immunotherapy that works with the patient’s own immune system to find and attack cancer cells. At the start of this treatment, immune cells called T cells are harvested by removing a patient’s blood through an IV line, cycling it through a machine that removes T cells, then cycling the blood back into the patient’s body. The T cells are then sent to a lab, where they are genetically altered so they have specific receptors (called chimeric antigen receptors, or CARs) on their surface. These receptors help the T cells attach to proteins on cancer cells and attack them. These modified T-cells are then infused back into the patient.
Local treatments are used to treat the tumor and not the rest of the body. They are generally used in solitary plasmacytomas, or symptomatic lesions of multiple myeloma, though each person’s individualized course of treatment may vary. Local treatments include:
Radiation therapy
Radiation therapy uses high-energy rays or particles to kill cancer cells. It may target specific areas of bone damaged by multiple myeloma that have not responded to chemotherapy or other drugs. It also may be used to treat solitary plasmacytomas. Multiple myeloma tumors are especially sensitive to radiation such that low doses are very effective.
The type of radiation most commonly used to treat multiple myeloma or solitary plasmacytoma is external beam radiation therapy, during which radiation is aimed at the cancer from outside the body. The procedure is similar to having a diagnostic x-ray, though it lasts longer. A course of treatment may last several weeks.
Surgery for multiple myeloma
Though surgery may be used to remove single plasmacytomas, it is not commonly used to treat multiple myeloma. Instead, it may be used to address issues such as weakened bones, spinal cord compression, or fractures that may be associated with multiple myeloma.
Supportive treatments for multiple myeloma
The goal of supportive treatments is to prevent or relieve symptoms associated with multiple myeloma rather than cure the cancer. These treatments aim to improve a patient’s quality of life and comfort, and may be used simultaneously with treatments whose goal is to cure the cancer. These may include treatments to help fight infection, treat anemia, or address physical, mental, or emotional symptoms that a patient may be experiencing.
The University of Colorado (CU) Cancer Center partners with UCHealth, Children’s Hospital Colorado, and Rocky Mountain Regional VA to provide clinical care. Please make an appointment with one of our clinical partners to be seen by a CU Cancer Center doctor.
UCHealth Cancer Care - Anschutz Medical Campus
1665 Aurora Court Anschutz Cancer Pavilion
Aurora, CO 80045
720-848-0300
UCHealth Cherry Creek Medical Center
100 Cook Street
Denver, CO 80206
720-848-0000
UCHealth Cancer Center - Highlands Ranch
1500 Park Central Drive
Highlands Ranch, CO 80129
720-516-1100
UCHealth Lone Tree Medical Center
9548 Park Meadows Drive
Lone Tree, CO 80124
720-848-2200
Children's Hospital Colorado:
13123 East 16th Avenue
Aurora, CO 80045
720-777-6740
Rocky Mountain Regional VA Medical Center:
1700 North Wheeling Street
Aurora, CO 80045-7211
303-399-8020
Latest in Blood Cancer from the Cancer Center
Loading items....
Information reviewed by Dan Sherbenou, MD, PhD, in July 2025.