Contact UCHealth
Kidney Cancer
Shared Content Block:
News feed -- crop images to square
Clinical Trials
Make a Gift
What Is Kidney Cancer?
Kidney cancer, also known as renal cell carcinoma, is cancer that begins in the kidneys when cells begin to grow out of control. The kidneys are bean-shaped organs located on both sides of the spine behind the other abdominal organs. The main job of kidneys is to remove excess water, salt, and other waste from the blood. The waste that is filtered by the kidneys becomes urine that collects in the center of each kidney in the renal pelvis and exits the kidneys through tubes called ureters. These tubes lead to the bladder.
According to the American Cancer Society, Kidney cancer is among the 10 most common cancers among men and women, with men (one in 43) being twice as likely as women (one in 73) to be diagnosed. Kidney cancer is more common among African Americans and American Indian/Alaska Natives. The median age of people diagnosed with kidney cancer is 64. The American Cancer Society estimates about 81,610 new cases of kidney cancer, about 52,380 in men and 29,230 in women, are diagnosed and about 14,390 people, 9,450 men and 4,940 women, die from the disease every year.
Renal cell carcinoma is the most common type of kidney cancer in adults, making up about nine out of every 10 kidney cancers diagnosed. Although rare, a solid kidney cancer tumor called Wilms tumor is the third most common type of solid tumor affecting children.
Kidney cancer rates have been rising since the 1990s; however, death rates have remained stable. One explanation for the increased number of cases diagnosed is the use of computerized tomography (CT) scans and other imaging techniques that can detect cancers that might have never been found otherwise.
Why Come to CU Cancer Center for Kidney Cancer
The CU Cancer Center is the only National Cancer Institute (NCI) Designated Comprehensive Cancer Center in Colorado and one of four in the Rocky Mountain region. Our doctors provide world-class, patient-centered care and have access to cutting-edge treatments not available at most other medical centers in the country. A multidisciplinary team can open the door for more treatment options, clinical trials, and a well-rounded care plan. Contact the Urology Multidisciplinary Clinic at 720-848-0181.
The CU Cancer Center is a member of the National Comprehensive Cancer Network (NCCN) advisory panels. The NCCN establishes guidelines for the diagnosis and treatment of all cancer types. Doctors all across the United States and throughout the world for use these guidelines as a reference.
The University of Colorado is a Von Hippel-Lindau (VHL) Alliance Clinical Care Center, recognized for dedication to a team approach and for additional depth of expertise and experience in treating VHL patients who have kidney and other VHL-associated tumors.
The CU Cancer Center offers kidney cancer patients the expertise of a team specializing in kidney cancer care, as well as cutting edge research through clinical trials that give patients more treatment options. Patients at the University of Colorado also have the added benefit of the entire institution and the collection supportive oncology teams behind them in their fight to overcome cancer.
For more information on pediatric kidney cancer, and to learn more about the care team and conditions treated, visit the pediatric Urologic Tumor Program and our Solid Tumor team at Children’s Hospital Colorado.
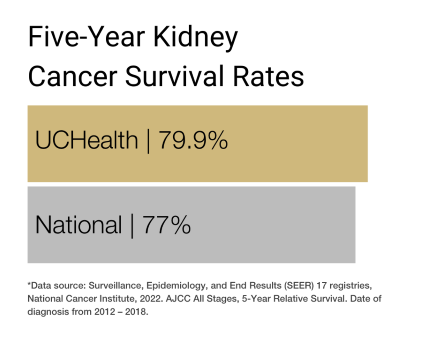
Our clinical partnership with UCHealth has produced survival rates higher than the state average for all stages of kidney cancer and other urologic cancers.
Types of Kidney Cancer
Renal cell carcinoma is the most common type of kidney cancer. Renal cell carcinoma usually occurs as a single tumor in a kidney, or two or more tumors in one or both kidneys. There are several subtypes of renal cell carcinoma, determined by the appearance of the cells from a biopsy. The renal cell carcinoma subtype determines the course of treatment for the patient.
There are two main types of kidney cancers; clear cell renal cell carcinomas and non-clear cell renal cell carcinomas.
Clear cell renal cell carcinoma is the most common subtype of renal cell carcinoma with seven out of 10 people with renal cell carcinoma having clear cell carcinoma. Under a microscope, clear cell renal cell carcinoma cells appear pale with clear cytoplasm.
Non-clear cell renal cell carcinomas have multiple subtypes, of which papillary renal cell carcinoma and chromophobe renal cell carcinoma are the most common.
- Papillary renal cell carcinoma is the second most common subtype of renal cell carcinoma, about one in 10 cases. These cancers appear finger-like.
- Chromophobe renal cell carcinoma accounts for about 5% of renal cell carcinomas. Like clear cell renal cell carcinoma, the cells of these cancers can be pale but are usually larger.
Rare types of renal cell carcinoma subtypes make up less than 1% of renal cell carcinomas.
- Collecting duct renal cell carcinoma.
- Multilocular cystic renal cell carcinoma.
- Medullary carcinoma.
- Mucinous tubular and spindle cell carcinoma.
- Neuroblastoma-associated renal cell carcinoma.
Other types of cancers can occur in the kidneys, but have a different biology than renal cell carcinoma and are treated differently.
Transitional cell carcinomas, also known as urothelial carcinomas, account for 5% to 10% of cancers in the kidneys. Transitional cell carcinomas start in the lining of the renal pelvis, which is made up of cells called transitional cells. These cells appear similar to cells found in the ureters and the bladder. Cancers that develop in the transitional cells look and behave like other urothelial carcinomas and are treated similar to bladder cancer.
Wilms tumor (nephroblastoma) occurs almost exclusively in children. They are the most common type of kidney cancer in children, making up about nine in 10 cases.
Renal sarcoma is a rare type of cancer that begins in the blood vessels or connective tissues of the kidneys. It accounts for less than 1% of kidney cancers.
Benign kidney tumors
Some kidney tumors are non-cancerous, meaning they do not metastasize or spread to other areas of the body and are easily treated by removal.
Angiomyolipomas are the most common type of benign kidney tumor. Angiomyolipomas are made up of different types of connective tissues (blood vessels, muscle, fat) and are more prevalent in women.
Oncocytomas are uncommon benign kidney tumors that can grow large and are more prevalent in men.
Causes of Kidney Cancer
Kidney cancer occurs when deoxyribonucleic acid (DNA) gets damaged or mutates (changes). DNA is a molecule in the cells that make up genes. Genes provide instructions to the cells, telling them when to grow, divide, and die. Kidney cancer forms when a cell’s DNA is damaged or altered, and the cells continue to grow and divide out of control where they aren’t needed.
Genetic mutations can be inherited or acquired. Inherited gene mutations run in families and increase the risk of developing kidney cancer. Acquired gene mutations are changes that occur over the course of a person’s lifetime and are not passed on. Most cases of kidney cancer are acquired DNA mutations rather than inherited.
Most cases of kidney cancers are acquired rather than inherited. The most common inherited kidney cancer is Von Hippel-Lindau (VHL) syndrome. VHL disease is caused by mutation of VHL, a tumor suppressing gene that would normally help keep cells from growing uncontrollably. When a VHL gene is mutated, it leads to the build-up of abnormal proteins that lead to abnormal cell growth. VHL syndrome is also associated with hemangioblastomas of the brain and spinal cord, pancreas tumors, in addition to kidney tumors.
In 2021, the FDA approved Belzutifan (Welireg) for the treatment of VHL-syndrome associated tumors. In 2023, Belzutifan (Welireg) received a second FDA approval for the treatment of metastatic renal cell carcinoma after prior immunotherapy and prior VEGFR inhibitor targeted therapy, regardless of VHL mutation status.
Other inherited conditions can lead to the development of kidney cancer:
- Hereditary leiomyomata and renal cell carcinoma (HLRCC) is caused by changes in the fumarate hydratase (FH) gene. Patients with HLRCC have papillary type II renal cell carcinoma, as well as leiomyomatosis in the skin and uterus.
- Birt-Hogg-Dube syndrome is an inherited condition in which patients have kidney cysts and kidney cancers in additions to skin tumors and lung cysts. Birt-Hogg-Dube syndrome is caused by mutations in the FLCN gene that creates a protein call folliculin.
- Hereditary papillary renal cell carcinoma (type I papillary RCC) is caused by alteration of the MET oncogene.
Some genetic tests can detect gene mutations associated with inherited syndromes. It is recommended to seek genetic testing and genetic counseling if there is a family history of kidney cancers linked to these syndromes.
Risk Factors for Kidney Cancer
While the cause of kidney cancer is not known for most patients, there are several factors that might increase the chance of developing kidney cancer. These risk factors include:
Age: The risk of developing kidney cancer increases with age.
Gender: Renal cell carcinoma is twice as common in men as in women.
Race: Renal cell carcinoma is slightly more common among African Americans than Caucasian people.
Smoking: People who smoke are at greater risk of developing kidney cancer than nonsmokers. The risk decreases after quitting.
Obesity: People who are overweight have a higher risk of developing renal cell carcinoma.
High blood pressure: People who have hypertension are at increased risk of developing kidney cancer.
Kidney disease: People with advanced kidney disease have a higher risk of developing renal cell carcinoma.
Family history of kidney cancer: People with close family members with kidney cancer have an increased risk. (See Von Hippel-Lindau)
Symptoms of Kidney Cancer
Kidney cancer does not usually cause symptoms in its early stages. Signs and symptoms that may develop include:
- Blood in the urine.
- Persistent lower back pain on one side.
- A mass or lump on the abdomen.
- Tiredness.
- Unexplained weight loss.
- Persistent fever not caused by an infection.
- Low red blood cell count.
Diagnosing Kidney Cancer
There are currently no recommended screening tests for kidney cancer for people at average risk of kidney cancer. Kidney cancers are often diagnosed when patients present with symptoms of back/flank pain or have blood noted on a urinalysis. Increasingly, kidney cancers are discovered incidentally when patients undergo abdominal imaging for other reasons.
People with inherited conditions like von Hippel-Lindau disease, which increases the risk of kidney cancer, are recommended to get regular imaging tests such as CT, MRI, or ultrasound starting at age 15. The age to start screening for kidney cancer varies from age 12 to age 30 depending on the specific inherited condition.
Tests for Kidney Cancer
If signs or symptoms of kidney cancer are evident, a doctor may recommend one or more of the following blood, urine, or imaging tests or procedures.
Blood and urine tests: Blood and urine tests cannot show if a person has kidney cancer; however, they can provide more details that can help lead to a cancer diagnosis.
Imaging tests: Ultrasound, X-ray, CT, MRI, and angiogram are imaging tests that allow doctors to create pictures of the inside of the body. They are done to look at suspicious areas, see if the cancer has spread, and help determine treatment.
- Ultrasound can find a mass in the kidney and show if it is solid or filled with fluid.
- A CT scan uses X-rays to take detailed images of the body and can provide information on the size, shape, and location of a kidney tumor.
- A CT-guided needle biopsy is a test that uses a CT to help guide a needle into the tumor to get a sample of cells.
- MRI scans use radio waves and magnets to take images of the body. MRIs can be used to look at the blood vessels to see if the cancer has grown into any of the major blood vessels in the abdomen.
- An angiogram is an X-ray test that uses a dye injected into an artery to look at the blood vessels that feed kidney tumors.
Biopsy: A biopsy is the removal of a small sample of tissue to be examined in a lab for cancerous cells. For the most part, imaging tests provide enough information for a surgeon to decide if an operation is needed. In some cases, a biopsy may be done to confirm the diagnosis.
Stages of Kidney Cancer
Once kidney cancer has been diagnosed, doctors will try to determine the stage of the cancer. The stage of the cancer describes how big a cancer is and if it has spread to lymph nodes and/or other organs. Knowing the stage of kidney cancer helps determine how best to treat it.
The staging system most commonly used for kidney cancer is the American Joint Committee on Cancer (AJCC) TNM system. The TNM system assesses the size of the tumor (T), if the tumor has spread to nearby lymph nodes (N), and if the tumor has spread (M-metastasized) to other sites of the body.
Kidney Cancer Stages
Stage 1: The tumor is 7 cm across or smaller, is only found in the kidney, and has not yet spread to the lymph nodes.
Stage 2: The tumor is larger than 7 cm across but is only found in the kidney and had not spread to the lymph nodes.
Stage 3: The tumor is growing into a major vein or the tissue of the kidney or may be outside the kidney but has not started growing into the adrenal gland or beyond the Gerota’s fascia (also known as renal fascia), is collagen-filled, fibrous connective tissue that encapsulates the kidneys and adrenal glands. The cancer may have spread to nearby lymph nodes.
Stage 4: The main tumor is growing beyond the Gerota’s fascia and may be growing into the adrenal gland. The tumor may be any size and may have grown outside the kidney and metastasize (spread) to nearby and distant lymph nodes, bone, or organs.
Treatments for Kidney Cancer
Treatment options for kidney cancer are tailored to each patient and depend on the stage of the cancer. Treatments for kidney cancer may include surgery, local ablative therapy, radiation, or systemic therapy (targeted therapy or immunotherapy).
Surgery for Kidney Cancer
Surgery is the main treatment for localized kidney cancers and sometimes metastatic kidney cancers. Surgery may be done to remove a portion of the kidney (called a partial nephrectomy) or the entire kidney (called a radical nephrectomy).
During a partial nephrectomy, the portion of the affected kidney with the tumor is removed, leaving the rest of the kidney behind. This procedure is usually a good option for kidney cancers that are less than 7 cm in size. This is the preferred treatment for patients with early-stage kidney cancer.
A radical nephrectomy is the removal of the whole kidney with or without removal of the attached adrenal gland or nearby lymph nodes, and the fatty tissue around the kidney. The body can function with just one kidney. Radical nephrectomies can be performed as open surgeries or using the minimally invasive techniques laparoscopic nephrectomy or robotic-assisted laparoscopic nephrectomy.
Laparoscopic nephrectomy: A long tube with a camera on the end, called a laparoscope, is inserted through ½-inch long incisions into the abdomen to allow the surgeon to see inside. The kidney is excised using special instruments and then removed through another incision.
Robotic-assisted laparoscopic nephrectomy: A procedure performed using a robotic system to do the laparoscopic surgery remotely. The surgeon controls the robotic arms from a panel near the operating table. The robotic system allows the surgeon to move the instruments more easily and with more precision.
Regional lymphadenectomy: During this procedure, nearby lymph nodes are removed to see if they contain cancer. This is often done during a radical nephrectomy.
Adrenalectomy: The removal of an adrenal gland. This is often performed as part of a radical nephrectomy.
Localized Treatments for Small Kidney Cancer Tumors
For patients with small kidney cancer tumors who are not candidates for surgery, local ablative therapies may be used to treat the cancers without removing them. Localized treatments include cryotherapy, radiofrequency ablation, and radiation therapy.
Cryotherapy uses liquid nitrogen inserted into the tumor through a probe to freeze cancer cells.
Radiofrequency ablation uses high-energy radio waves through a probe to heat up the tumor and kill the cancer cells.
Radiation therapy is a treatment that uses high-energy rays to destroy cancer cells. Stereotactic body radiation therapy (SBRT) is an option for treating small kidney cancers and small, isolated areas of metastases. External beam therapy (EBRT) is most commonly used to treat kidney cancer that has metastasized to other organs and is causing symptoms.
Systemic Therapies for Kidney Cancer
Systemic therapies are treatments either taken as a pill or given as an infusion through a vein to help treat kidney cancer cells that have entered the bloodstream and spread to other areas of the body. Traditional chemotherapy treatments that are used to treat other types of cancers generally do not work for kidney cancer. Instead, systemic therapies for kidney cancer include targeted therapies and immunotherapies. Depending on the situation, targeted therapy and immunotherapy may be given as a single drug or in combination.
Targeted Drug Therapy for Kidney Cancer
Targeted drugs are used to shrink or slow the growth of kidney cancers. They can sometimes be used after surgery in people at high risk of recurrence. In advanced or metastatic cases of kidney cancer, targeted drugs are used to block blood vessels that feed cancers (angiogenesis) or block proteins that help tumors grow (tyrosine kinases).
Drugs that target tumor blood vessel growth include:
- Sunitinib (Sutent®) blocks both angiogenesis and tyrosine kinases in cancer cells. This drug is taken as a pill daily, for four weeks on and two weeks off. Sunitinib can also be used after surgery for patients at risk of recurrence.
- Sorafenib (Nexavar®) blocks tyrosine kinases by attacking both blood vessel growth and proteins that promote cancer cell growth. Sorafenib is taken as pills twice a day.
- Pazopanib (Votrient®) blocks tyrosine kinases involved in cancer cell growth and blood vessel growth. Pazopanib is taken as pills once a day.
- Cabozantinib (Cabometyx®) blocks several types of tyrosine kinases and is taken as a pill once a day.
- Lenvatinib (Lenvima®) is a kinase inhibitor that blocks tumors from forming new blood vessels. This drug is taken once a day.
- Bevacizumab (Avastin®) is an IV drug that works to slow new blood vessel growth. It is given through a vein once every two or three weeks.
- Axitinib (Inlyta®) inhibits several types of tyrosine kinases and is a pill taken twice a day.
- Tivozanib (Fotivda®) blocks several types of tyrosine kinases involved in cancer cell growth and the formation of new blood vessels. This drug is taken as a pill daily for three weeks on and one week off.
Drugs that target the mammalian target of rapamycin (mTOR) protein which regulates cell growth, survival, metabolism, and immunity include:
- Temsirolimus (Torisel®) blocks the protein mTOR which helps cells grow and divide. This drug is given as an IV infusion once a week.
- Everolimus (Afinitor®) blocks the mTOR protein and is taken as a pill once a day.
Drugs that target hypoxia inducible factor 2-alpha protein (HIF-a) which regulates oxygen sensing and survival of renal cell carcinomas include:
- Belzutifan (Welireg®) blocks HIF-2a and is taken as a pill once a day.
Immunotherapy for Kidney Cancer
Immunotherapy uses drugs to train the immune system to enhance the body’s ability to fight cancer. This is achieved by turning off “checkpoint” proteins on immune cells to start an immune response against the cancer cells.
PD-1 Inhibitors
Pembrolizumab (Keytruda®) and Nivolumab (Opdivo®) are drugs that target PD-1, a protein on T cells, which normally keep cells from attacking other cells in the body. Blocking PD-1 helps boost the immune response against kidney cancer cells to shrink the tumor’s growth and keeps the cancer from spreading further to other places in the body. Both pembrolizumab and nivolumab are approved for the treatment of kidney cancers. Pembrolizumab is also approved for adjuvant treatment for high-risk, non-metastatic kidney cancers.
PDL-1 Inhibitors
Avelumab (Bavencio®) targets PD-1L, a protein found on tumor cells and immune cells. Blocking the PD-1L protein helps boost the immune response against the cancer cells.
CTLA-4 Inhibitors
Ipilimumab (Yervoy®) boosts the immune response by blocking CTLA-4, a protein on T cells that keeps them in check.
Clinical Trials for Kidney Cancer
Clinical trials are an important option for patients with kidney cancer to gain access to cutting-edge treatment options. The NCCN encourages all patients to consider clinical trials whenever they are available and suitable for their situation.
The University of Colorado (CU) Cancer Center partners with UCHealth, Children’s Hospital Colorado, and Rocky Mountain Regional VA to provide clinical care. Please make an appointment with one of our clinical partners to be seen by a CU Cancer Center doctor.
UCHealth Cancer Care - Anschutz Medical Campus
1665 Aurora Court Anschutz Cancer Pavilion
Aurora, CO 80045
720-848-0300
UCHealth Cherry Creek Medical Center
100 Cook Street
Denver, CO 80206
720-848-0000
UCHealth Cancer Center - Highlands Ranch
1500 Park Central Drive
Highlands Ranch, CO 80129
720-516-1100
UCHealth Lone Tree Medical Center
9548 Park Meadows Drive
Lone Tree, CO 80124
720-848-2200
Children's Hospital Colorado:
13123 East 16th Avenue
Aurora, CO 80045
720-777-6740
Rocky Mountain Regional VA Medical Center:
1700 North Wheeling Street
Aurora, CO 80045-7211
303-399-8020
Latest in Kidney Cancer from the Cancer Center
Loading items....
Information reviewed by Elaine Lam, MD, in July 2025.