Contact UCHealth
Uterine Cancer (Endometrial Cancer or Uterine Sarcoma)
Clinical Trials
Make a Gift
What Is Uterine Cancer?
Uterine cancer is a cancer that starts in the uterus, the hollow, pear-shaped pelvic organ where fetal development occurs. There are two primary types of uterine cancer: endometrial cancer, which starts in cells in the inner lining of the uterus, known as the endometrium; and uterine sarcoma, which starts in the muscle (myometrium) and supporting tissue of the uterus. Endometrial cancer is much more common than uterine sarcoma.
Uterine and Endometrial Cancer Prognosis and Survival Rates
Uterine cancer prognosis depends on the type of cancer and the stage at which it is diagnosed.
Endometrial cancer is the most common cancer of the female reproductive system. The American Cancer Society estimates that in 2022, around 65,950 new cases of uterine cancer (including endometrial cancer and uterine sarcoma) will be diagnosed, and around 12,550 women will die from cancers of the uterus.
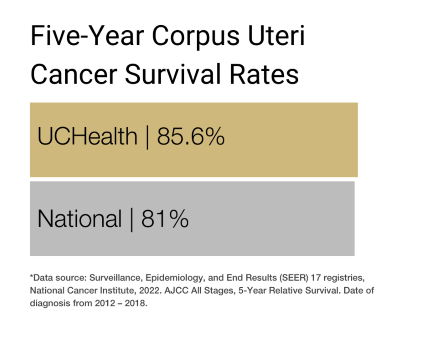
The five-year survival rate for endometrial cancer is 81%.
Uterine sarcoma is much rarer, accounting for around 2% to 5% of all uterine cancers in the United States, according to the American Cancer Society. Thanks to advances in treatment, the five-year survival rate for uterine sarcoma ranges from 39% to 98%, depending on the type of sarcoma and how far it has spread in the body, if at all.
Why Come to CU Cancer Center for Uterine and Endometrial Cancer
As the only National Cancer Institute-designated Comprehensive Cancer Center in Colorado and one of only four in the Rocky Mountain region, the University of Colorado Cancer Center has doctors who provide cutting-edge, patient-centered uterine and endometrial cancer care, and researchers focused on diagnostic and therapeutic innovations.
The CU Cancer Center is one of the first and only centers in the country to perform comprehensive molecular testing on every endometrial cancer case. These molecular results are essential to determining a patient’s prognosis and providing a personalized treatment plan to achieve the best outcomes.
There are numerous uterine cancer clinical trials being conducted by CU Cancer Center members at any time. These trials offer patients options to traditional uterine cancer treatment and can result in remission or increased life spans.
>> CU Cancer Center Members Use National Patient Database to Aid in Endometrial Cancer Research
Types of Uterine Cancer
Uterine cancers can be of two types: endometrial cancer (common) and uterine sarcoma (rare).
Endometrial cancer
Endometrial cancer begins in the layer of cells that form the lining (endometrium) of the uterus. There are six primary types of endometrial cancer:
- Adenocarcinoma (most endometrial cancers are adenocarcinomas).
- Serous carcinoma.
- Uterine carcinosarcoma.
- Small cell carcinoma.
- Transitional carcinoma.
- Squamous cell carcinoma.
Uterine sarcoma
Uterine sarcoma is largely categorized into four types:
- Uterine leiomyosarcoma (LMS) is the most common type of uterine sarcoma. It starts in the muscle layer of the uterus known as the myometrium.
- Endometrial stromal sarcomas (ESS) are tumors that form in the connective tissue (known as the stroma) of the uterine lining (the endometrium).
- Adenosarcoma is a type of sarcoma in which normal gland cells are mixed with cancer cells of the stroma.
- Undifferentiated sarcoma can form in the endometrium or the myometrium.
Risk Factors for Uterine Cancer
Uterine cancer has multiple risk factors: behaviors or conditions that increase a person’s chances of getting a disease such as cancer. Risk factors for uterine cancer include:
Endometrial cancer risk factors
- Previous radiation therapy to the pelvis for conditions such as cervical cancer or rectal cancer.
- Obesity.
- History of endometrial hyperplasia.
- Long menstruation span caused by early menstruation (before 12) or late menopause (after 50).
- Nulliparity (never having been pregnant).
- Poor diet, especially a diet high in animal fat.
- Medications or other factors that affect hormone levels, including taking tamoxifen, birth control pills, or estrogen; having polycystic ovarian syndrome; and certain types of ovarian tumors.
- Hereditary cancer syndromes with risk of uterine cancer (i.e., Lynch Syndrome).
- Family history of endometrial or colorectal cancer.
Uterine sarcoma risk factors
- Previous radiation therapy to the pelvis for conditions such as cervical cancer or rectal cancer.
- Hereditary syndromes including hereditary leiomyomatosis and renal cell carcinoma (HLRCC) and retinoblastoma.
- Taking tamoxifen to treat or prevent breast cancer.
- Age: Uterine sarcomas occur most often in people 40 and older.
Symptoms of Uterine Cancer
Uterine cancer can usually be treated successfully if it is diagnosed before the cancer has spread to distant parts of the body.
Symptoms of uterine cancer include:
- Abnormal vaginal bleeding or spotting (most common).
- Pain or a mass in the pelvis.
- Weight loss.
- Frequent urination.
- Constipation.
Screening for Uterine Cancer
Screening is used to look for cancer before a person shows any symptoms of the disease. There are no standard screenings for uterine or endometrial cancer. The Pap smear does not check for uterine cancer; it is a screening test for cervical cancer. Abnormal vaginal bleeding should be evaluated by a doctor as soon as possible.
Diagnosing Uterine Cancer
Based on a patient’s symptoms and after an initial physical examination, a doctor may order certain tests to determine whether the patient has uterine cancer. Though testing procedures can vary based on the type of uterine cancer the doctor is looking for, common tests for uterine cancer include:
Biopsy: During a biopsy, a doctor extracts a sample of tissue from the endometrium. These are often performed in clinic and sent to a laboratory for analysis by a pathologist to determine whether the cells in the sample are cancerous. In some cases, a dilation and curettage (D&C) must be performed in the operating room to obtain additional tissue.
Hysteroscopy: This procedure uses a very small telescope or camera, inserted through the cervix, to view the lining of the uterus. Doctors can look for cancers or polyps and biopsy them if necessary.
Magnetic resonance imaging (MRI): An MRI uses radio waves and magnetic fields to produce detailed images of the body. MRI scans can show if endometrial cancer has spread into the body of the uterus and if so, how far.
Computed tomography (CT or CAT) scan: A CT scan uses X-rays to take detailed images of the body and can help determine if cancer has spread to other organs or come back after treatment.
Positron emission tomography (PET) scan: A slightly radioactive form of sugar is injected into the blood, where it is taken in by cells in the body. Since cancer cells grow faster than normal cells, they take in larger amounts of the sugar. Doctors use PET scans to look for possible areas of cancer spread, and to determine if suspicious areas seen in other imaging tests are cancer or not. PET scans are not frequently used for uterine cancer.
Ultrasound: This imaging test uses sound waves to create pictures of internal organs or masses. Ultrasound can be used to look for a mass inside the uterus.
Hysterectomy: Some uterine cancers cannot be biopsied or diagnosed prior to surgery. In these cases, the uterus has to be removed in order to make the diagnosis of cancer. The surgery to remove the uterus is called a hysterectomy and includes removal of the uterus, cervix, fallopian tubes, and possibly the ovaries depending on a patient’s age and cancer type.
Lymph node dissection: This operation removes lymph nodes from the pelvis and the area around the aorta. The nodes are then examined to look for cancer cells that have spread from the uterus. This procedure is done at the time of hysterectomy.
Pelvic washing: One way of finding uterine cancer cells is to “wash” the pelvic and abdominal cavities with a saline solution. The solution is then sent to a lab, where it is examined to look for cancer cells. This procedure is done at the time of hysterectomy.
Stages of Uterine Cancer
After diagnosing the presence of uterine cancer, the doctor will identify the stage of the disease. The stage is determined by several factors, including where exactly the disease formed, how extensive it is, and whether and how much it has spread. The stage of uterine cancer is usually determined surgically, meaning at time of hysterectomy/removal of uterus, lymph node dissection, and pelvic washings.
Many of the same tests used to diagnose uterine cancer can also be used to help determine the stage, including biopsies, X-rays, CT/CAT scans, and PET scans.
Doctors typically use the TNM system to determine the stage of uterine cancer. The TNM system assesses the size and extent of the tumor (T) and whether it has ulcerated; whether the cancer has spread to nearby lymph nodes (N); and the presence and extent of metastasis (M) to distant lymph nodes, bones, and organs.
After the TNM assessment, the doctor will assign an overall stage number from I to IV, which can be further broken down based on the size of the original tumor and the extent to which the cancer has spread. In general, the lower the stage the better the prognosis and treatment options.
Leiomyosarcoma and Endometrial Stromal Sarcoma Stages
Stage I: The tumor is limited to the uterus.
Stage IA: The tumor is less than 5 centimeters.
Stage IB: The tumor is more than 5 centimeters.
Stage II: The tumor extends beyond the uterus and is contained within the pelvis.
Stage IIA: There is adnexal involvement.
Stage IIB: There is involvement of other pelvic tissues.
Stage III: The tumor is invading abdominal tissues and not just protruding into the abdomen.
Stage IIIA: Cancer is in one additional site.
Stage IIIB: Cancer is in more than one additional site.
Stage IIIC: Cancer has spread to the pelvic and/or para-aortic lymph nodes.
Stage IVA: The tumor has invaded the bladder and/or rectum.
Stage IVB: The cancer has spread to distant sites in the body.
Adenosarcoma Stages
Stage I: The tumor is limited to the uterus.
Stage IA: The tumor is limited to the endometrium/endocervix with no myometrial invasion.
Stage IB: The tumor is less than or equal to half myometrial invasion.
Stage IC: The tumor is more than half myometrial invasion.
Stage II: The tumor extends to the pelvis.
Stage IIA: There is adnexal involvement.
Stage IIB: The tumor extends to extrauterine pelvic tissue.
Stage III: The tumor is invading abdominal tissues and not just protruding into the abdomen.
Stage IIIA: Cancer is in one additional site.
Stage IIIB: Cancer is in more than one additional site.
Stage IIIC: Cancer has spread to the pelvic and/or para-aortic lymph nodes.
Stage IVA: The tumor has invaded the bladder and/or rectum.
Stage IVB: The cancer has spread to distant sites in the body.
Treatments for Uterine Cancer
The treatment for uterine cancer is customized to each patient and depends on the stage at which the patient is diagnosed, and the patient’s general health.
Uterine cancer care teams may include multiple health care specialists, including primary care providers, gynecologists, gynecologic oncologists, medical oncologists, hematologists, and radiation oncologists, as well as nurse practitioners, physician assistants, nurses, psychologists, social workers, and rehabilitation specialists. CU Cancer Center doctors offer specialized care for patients with uterine cancer.
Treatments for uterine cancer include surgery, radiation therapy, chemotherapy, immunotherapy, and targeted drug therapy. Patients may receive one or more of these treatments in combination. Some patients may also be eligible to participate in clinical trials — doctor-led research studies of new or experimental procedures or treatments.
Surgery for Uterine Cancer
The primary treatment for endometrial cancer is a hysterectomy — surgery to remove the uterus and cervix. A hysterectomy can be performed through a large incision in the abdomen or using laparoscopic surgery which is less invasive.
Another surgery commonly used to treat uterine cancer is a bilateral salpingo-oophorectomy, an operation to remove both fallopian tubes and both ovaries. The operation is typically performed at the same time as a hysterectomy, depending on a patient’s age and cancer type.
Radiation Therapy for Uterine Cancer
Radiation therapy uses high-powered energy to kill cancer cells. A doctor who specializes in radiation therapy to treat cancer is a radiation oncologist. The two main types of radiation therapy used to treat uterine cancer are external beam radiation and brachytherapy.
External-beam radiation therapy (EBRT) is the most common radiation treatment and uses a machine located outside the body to focus a beam of X-rays on the area with the cancer.
Brachytherapy, or internal radiation therapy places radioactive materials inside the body to provide a localized treatment. In the case of uterine cancer, radioactive materials are placed into a cylinder that is inserted into the vagina. Treatments typically take less than an hour and are given daily or weekly for at least three doses.
Chemotherapy for Uterine Cancer
Chemotherapy uses drugs to kill rapidly growing cancer cells. Drugs are either injected into a vein or taken orally. Depending on the type of uterine cancer, chemotherapy may be combined with immunotherapy or followed by radiation therapy.
Immunotherapy for Uterine Cancer
Sometimes the body’s immune system does not attack cancer because cancer cells produce proteins that help them hide from immune system cells. Immunotherapy, also called biologic therapy, boosts the patient’s immune system to help it attack and destroy cancer cells.
Immune checkpoint inhibitors or checkpoint blockade therapies are drugs that target the body’s checkpoint proteins, helping restore the immune system’s natural defenses against cancer cells. Checkpoint inhibitors used to treat uterine cancer include pembrolizumab and dostarlimab.
Targeted Drug Therapy for Uterine Cancer
Targeted therapy focuses on the specific genes, proteins, or tissue environments that contribute to uterine cancer, limiting damage to non-cancerous cells and tissues.
The most common targeted drug therapies for uterine cancer include:
Kinase inhibitors and angiogenesis inhibitors work by preventing tumors from creating new blood vessels, and by targeting proteins that allow cancer cells to grow.
mTOR inhibitors block the activity of a specific protein in cancer cells that helps them grow and spread.
Hormone Therapy for Uterine Cancer
Hormone therapy uses medication to block or change the levels of certain hormones to slow the growth of uterine cancer. It is typically used to treat advanced-stage uterine cancer or uterine cancer that has recurred after treatment. The most common hormone treatments for uterine cancer include:
Progestins slow the growth of uterine cancer cells.
Aromatase inhibitors stop the production of estrogen in the adrenal glands and fatty tissues — the most common sites of estrogen production after menopause.
The University of Colorado (CU) Cancer Center partners with UCHealth, Children’s Hospital Colorado, and Rocky Mountain Regional VA to provide clinical care. Please make an appointment with one of our clinical partners to be seen by a CU Cancer Center doctor.
UCHealth Cancer Care - Anschutz Medical Campus
1665 Aurora Court Anschutz Cancer Pavilion
Aurora, CO 80045
720-848-0300
UCHealth Cherry Creek Medical Center
100 Cook Street
Denver, CO 80206
720-848-0000
UCHealth Cancer Center - Highlands Ranch
1500 Park Central Drive
Highlands Ranch, CO 80129
720-516-1100
UCHealth Lone Tree Medical Center
9548 Park Meadows Drive
Lone Tree, CO 80124
720-848-2200
Children's Hospital Colorado:
13123 East 16th Avenue
Aurora, CO 80045
720-777-6740
Rocky Mountain Regional VA Medical Center:
1700 North Wheeling Street
Aurora, CO 80045-7211
303-399-8020
Latest News from the Cancer Center
Loading items....
Information reviewed by Marisa Moroney, MD, in January 2024.