Contact UCHealth
Cervical Cancer
Shared Content Block:
News feed -- crop images to square
Clinical Trials
Make a Gift
What Is Cervical Cancer?
Cervical cancer is a cancerous growth that starts in the cells of the cervix. The cervix is part of a woman’s reproductive system – it is the lower, narrow end of the uterus and connects the uterus to the vagina.
Cervical cancer is one of the most common causes of cancer death among women outside of the US. While it is less common in the US, according to the American Cancer Society, there are more than 13,900 new cases will be diagnosed in 2023 and an estimated 4,310 women will die of the disease. However, cervical cancer also is one of the most preventable types of cancer due to screening tests and vaccinations for the human papillomavirus (HPV). HPV is a sexually transmitted infection that is very common among sexually active men and women, and it is the driver for almost all cervical cancers.
Pap tests collect cells from the cervix and can detect cervical pre-cancer before it becomes cancerous. Doctors recommend that women start getting Pap tests at age 21. Women who have symptoms of bleeding between periods, pelvic pain, or discomfort or bleeding with sex should discuss these symptoms with their doctor and have a pelvic examination immediately.
There are several vaccines against the strains of HPV that cause cervical cancer, and getting vaccinated can prevent cervical cancer from forming. These vaccinations are recommended for EVERYONE, girls and boys, as early as 9 years old. Ideally, this occurs before they become sexually active. Vaccination is safe and available for everyone up to age 45 and should be discussed with their physician.
Cervical cancer is managed with surgery to remove the cervix only when it is stage 1. For anything more than stage 1 disease, surgery to remove the uterus and cervix is not used and both chemotherapy and radiation are typically needed. Like many cancers, if left untreated or undiagnosed, cervical cancer can spread to other parts of the body over time. This process is called metastasis and can be life threatening.
Cervical Cancer Prognosis and Survival Rates
Cervical cancer is most often diagnosed in women who are ages 35 and 44, and the average age at diagnosis is 50. It rarely is diagnosed in women younger than 20. However, even as women age, the risk of cervical cancer is still present. More than 20% of cervical cancer cases are diagnosed in women older than 65. Women who have been getting regular Pap screening tests for cervical cancer before they were 65 are very infrequently diagnosed with the disease.
Prognosis for cervical cancer may depend on factors that include:
- the stage at which the disease is diagnosed, including the size of the tumor and whether the cancer has spread beyond the cervix.
- the type of cervical cancer.
- a woman’s age and overall health.
- whether a woman has HIV or is otherwise immunocompromised.
- whether a woman is receiving a first-time diagnosis or the cancer has recurred.
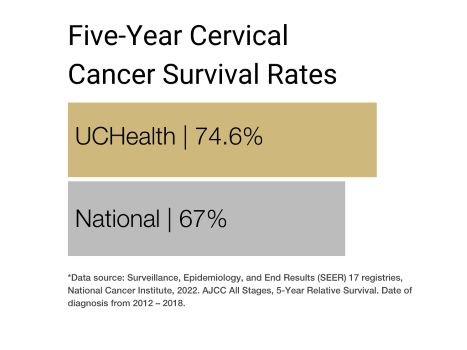
Cervical cancer survival rates are expressed in terms of five-year relative survival rate, which expresses what percent of people with the same type and stage of cervical cancer are alive five years after their cancer diagnosis, compared with people in the overall population. The five-year relative survival rates for cervical cancer are:
- When cervical cancer is diagnosed at an early stage, the five-year relative survival rate is 91%.
- When cervical cancer is diagnosed after it has spread to nearby tissues, organs, or lymph nodes, the five-year relative survival rate is 60%.
- When cervical cancer is diagnosed after it has spread to a distant part of the body, the five-year relative survival rate is 19%.
- The five-year relative survival rate for all people with cervical cancer is 67%.
However, it is important to remember that each woman is different and responses to treatment can vary widely. Each year, doctors and researchers are developing better treatments for cervical cancer, but the effects of newer and better treatments may not be reflected in current five-year relative survival rates.
Why Come to CU Cancer Center for Cervical Cancer
The University of Colorado Cancer Center's gynecologic oncology team are national leaders in patient care, including offering patients the latest technologies and treatment options. They are members of multidisciplinary treatment teams incorporating not only expertise in gynecologic oncology which includes chemotherapy and surgery, but also radiation oncology, radiology, social work, nutrition, finance support, and many other specialties so patients receive holistic, unified care.
Research has shown that gynecologic cancer patients have better treatment outcomes and survival rates if they're seen by a gynecologic oncologist, especially at the beginning of treatment. CU Cancer Center also offers access to cutting edge science through clinical trials.
The University of Colorado Cancer Center is one of only 33 centers in the country to qualify as a NCCN-designated cancer center. The National Comprehensive Cancer Network (NCCN) is an alliance of the nation's leading cancer centers, dedicated to providing expert patient care.
Types of Cervical Cancer
The main types of cervical cancers are squamous cell carcinoma and adenocarcinoma.
Most cervical cancers are squamous cell carcinomas, which develop from cells in the ectocervix, or the outer part of the cervix that a doctor can see during a speculum exam. Squamous cell carcinomas most often begin in the transformation zone, which is the area where the ectocervix joins the endocervix — the opening of the cervix that leads to the uterus.
Adenocarcinomas are cancers that develop from glandular cells. Cervical adenocarcinoma develops from the mucus-producing gland cells of the endocervix.
Much less commonly, a very few cervical cancers have features of both squamous cell carcinomas and adenocarcinomas. These are called adenosquamous carcinomas or mixed carcinomas.
Although almost all cervical cancers are either squamous cell carcinomas or adenocarcinomas, other types of cancer also can develop in the cervix. These other types — including melanoma, sarcoma, and lymphoma — occur more commonly in other parts of the body.
Risk Factors for Cervical Cancer
There are several risk factors that can increase a woman’s chance of developing cervical cancer, including:
- HPV infection.
- Smoking.
- Having a weakened immune system, including having HIV or taking medicines to suppress the immune system (steroids).
It is important to remember that while these risk factors can increase the odds of developing cervical cancer, many women with one or several of these risk factors do not develop the disease. It is also important to understand the cervical cancer IS NOT inherited, so a family member having cervical cancer does not place you at risk.
What can you do to decrease your risk of cervical cancer?
It is important to focus on addressing the risk factors that can be affected by behavior change, including:
- Do not smoke.
- Use condoms during sex.
- Minimize the number of sexual partners you have.
- Get Pap smears.
- Consume a well-balanced diet.
Symptoms of Cervical Cancer
Unfortunately, early stages of cervical cancers and pre-cancers often have no symptoms. The most common symptoms are:
- Abnormal vaginal bleeding, such as bleeding after vaginal sex, bleeding after menopause, bleeding and spotting between periods, or having periods that are longer or heavier than usual.
- An unusual discharge from the vagina, which may contain some blood and may occur between periods or after menopause.
- Pain during sex.
- Pain in the pelvic region.
Signs and symptoms of more advanced cervical cancer may include:
- Swelling of the legs.
- Shotting pain down the back of the legs.
- Problems urinating or having a bowel movement.
- Blood in the urine.
Though some of these symptoms may also by caused by conditions or diseases other than cervical cancer, they nevertheless are of great concern and a woman having any of them should consult a health care professional right away.
Diagnosing Cervical Cancer
Finding cervical cancer often begins with abnormal results from an HPV or Pap test. Because both are screening tests rather than diagnostic tests, they cannot determine whether a woman has cervical cancer. Generally, abnormal results from either test will lead a health care provider to do follow-up tests to determine whether a woman has cervical cancer or pre-cancer.
This follow-up to abnormal HPV or Pap test results may include:
A medical history and physical exam, during which a health care provider may ask for information related to risk factors and symptoms of cervical cancer. A complete physical exam will help evaluate a woman’s general state of health and may include feeling lymph nodes for signs that the cancer has spread.
Coloscopy, which is a procedure during which a doctor examines the cervix with a coloscope, an instrument that magnifies the surface of the cervix. A doctor places a speculum in the vagina and applies a vinegar-solution to the cervix to help them temporarily better see any areas of concern. They will then look through the colposcope, which is like a giant pair of binoculars, and decide if a biopsy is needed.
Cervical biopsy in the office, which includes several types:
- Colposcopic biopsy, during which the cervix is examined with a colposcope to find the abnormal areas. A very small section of the abnormal area on the surface of the cervix is removed using biopsy forceps, and a woman may experience mild cramping, brief pain, and some slight bleeding afterward.
- Endocervical curettage, or endocervical scraping, during which a narrow instrument is inserted into the endocervix, or the part of the cervix closest to the uterus and scrapes the inside of the canal to remove some of the tissue, which is then sent to a lab. After this procedure, women may feel a cramping pain, and they may also have some light bleeding.
Cervical excision in the office or operating room:
- LEEP, or loop electrosurgical excision procedure, is a D-shaped piece of cervix that is removed in either the office or in the operating room. The base of the cone is formed by the exocervix, or outer part of the cervix, and the apex of the cone is from the endocervical canal. The tissue removed in the LEEP includes the transformation zone, which is the border between the exocervix and endocervix, where cervical pre-cancers and cancers are most likely to start.
- Cone biopsy, also known as conization, is a procedure during which a doctor removes a cone-shaped piece of tissue from the cervix. This is done in the operating room. The base of the cone is formed by the exocervix, or outer part of the cervix, and the apex of the cone is from the endocervical canal. The tissue removed in the cone includes the transformation zone, which is the border between the exocervix and endocervix, where cervical pre-cancers and cancers are most likely to start. It is different than a LEEP in that it samples the endocervical canal more deeply, particularly important for an adenocarcinoma-in-situ (precancer). A cone biopsy can also be used as a treatment to completely remove many pre-cancers and some very early cancers.
If any of these follow-up tests indicate that a woman has cervical cancer, a doctor may perform further tests to determine how far the cancer has spread. These may include a chest x-ray, CT scan, MRI, PET scan, or intravenous urography, which is an x-ray of the urinary system.
Stages of Cervical Cancer
Staging cervical cancer may include determining how far the cancer has grown into the cervix, whether the cancer has spread to nearby structures, and whether it has spready to nearby lymph nodes or distant organs.
Health care professionals study the results of exams and tests to determine the tumor’s size and how deeply it has invaded tissues in and around the cervix, and whether it has spready to distant areas of the body.
For cervical cancer, the International Federation of Gynecology and Obstetrics (FIGO) guidelines are most commonly used for staging. Staging cervical cancer using the FIGO incorporates results from a doctor’s physical exam, biopsies, imaging tests, and a few other tests that are done in some cases. It is not based on what is found during surgery.
Cervical cancer stages range from stage 1 to stage 4, and as a rule the lower the stage, the less the cancer has spread. A higher number such as stage 4 indicates that the cancer has spread to other parts of the body; however, cervical cancer staging can be complex, so it’s important to ask health care providers for explanation and clarification.
Each stage of cervical cancer is divided into further substages:
Stage 1: The cancer cells have grown from the surface of the cervix into deeper tissues of the cervix but have not spread to nearby lymph nodes or distant areas of the body.
- Stage 1A: There is a very small amount of cancer, which can only be seen only under a microscope. The cancer has not spread to nearby lymph nodes or distant areas of the body.
- Stage 1A1: The area of cancer can only be seen with a microscope and is less than three millimeters, or about 1/8 inch, deep.
- Stage 1A2: The area of cancer can only be seen with a microscope and is between three to five millimeters deep, or about 1/5 inch.
- Stage 1B: The cancer has spread deeper than five millimeters, or about 1/5 inch, but is limited to the cervix.
- Stage 1B1: The cancer is deeper than five millimeters, or about 1/5 inch, but is not more than two centimeters, or about 4/5 inch, in size.
- Stage 1B2: The cancer is at least two centimeters in size but is not larger than four centimeters.
- Stage 1B3: The cancer is at least four centimeters in size but is limited to the cervix.
Stage 2: The cancer has grown beyond the cervix and uterus but hasn't spread to the walls of the pelvis or the lower part of the vagina. It has not spread to nearby lymph nodes or distant areas of the body.
- Stage 2A: The cancer has grown beyond the cervix and uterus but has not spread into the tissues next to the cervix, which are called the parametria.
- Stage 2A1: The cancer is not larger than four centimeters, or about 1 3/5 inches.
- Stage 2A2: The cancer is four centimeters or larger.
- Stage 2B: The cancer has grown beyond the cervix and uterus and has spread into the parametria (the connective/supporting tissue to the sides of the cervix). It has not spread to nearby lymph nodes or distant sites in the body.
Stage 3: The cancer has spread to the lower part of the vagina or the walls of the pelvis. The cancer may be blocking the tubes that carry urine from the kidneys to the bladder, called ureters. It might or might not have spread to nearby lymph nodes but has not spread to distant sites.
- Stage 3A: The cancer has spread to the lower part of the vagina but not the walls of the pelvis. It has not spread to nearby lymph nodes nor to distant areas of the body.
- Stage 3B: The cancer has grown into the walls of the pelvis and/or is blocking one or both ureters, causing kidney problems called hydronephrosis. It has not spread to nearby lymph nodes or to distant parts of the body.
- Stage 3C: The tumor may be any size and imaging tests or a biopsy show it has spread to nearby pelvic lymph nodes (stage IIIC1) or to para-aortic lymph nodes (stage IIIC2). It has not spread to distant sites in the body.
Stage 4: The cancer has grown into the bladder or rectum or to far away organs like the lungs or bones.
- Stage 4A: The cancer has spread to the bladder or rectum, or it is growing outside of the pelvis.
- Stage 4B: The cancer has spread to distant organs outside the pelvic area, such as distant lymph nodes, lungs, or bones.
Treatments for Cervical Cancer
Women who are diagnosed with cervical cancer have multiple treatment options and can work with their care teams to determine which treatment is most appropriate. Factors influencing treatment may include a woman’s age, overall health, and personal preferences.
Surgery for cervical cancer
Surgery is common treatment option that not only can be used to treat cervical cancer, but to diagnose it and determine how far it has spread.
For pre-cancers of the cervix, two common surgical procedures are ablation, which destroys cervical tissue with cold temperatures or a laser rather than removing it; and excisional surgery, also called conization or LEEP, which cuts out and removes pre-cancer.
Surgeries for invasive cervical cancer may include a simple or radical hysterectomy, or trachelectomy. During a simple hysterectomy, a surgeon removes the body of the uterus and the cervix, but not the structures next to the uterus or the vagina. In a radical hysterectomy, the surgeon removes the uterus as well as the tissues next to the uterus, the cervix, and the upper part of the vagina next to the cervix. The ovaries are not removed unless there is some other medical reason to do so. Sampling of the lymph nodes that drain the cervix depends on the type and size of the cancer.
If a cancer is small and a woman desires to preserve the ability to have future children, there are surgical options to accommodate this. These include conization or possible trachelectomy. During a trachelectomy, the surgeon removes the cervix and possibly the upper part of the vagina but not the body of the uterus. The uterus and vagina are then reconnected. The surgeon then places a permanent "purse-string" stitch inside the uterine cavity to keep the opening of the uterus closed, the way the cervix normally would. This surgery allows women to be treated without losing their ability to have children and is done either through the vagina or the abdomen, and the lymph nodes draining the cervix are sampled as well.
Radiation therapy for cervical cancer
Radiation therapy uses high-energy x-rays to kill cancer cells. Depending on the stage of the cervical cancer, radiation therapy may be used as part of the main treatment, or concurrently with chemotherapy. Radiation therapy may be used to treat cervical cancers that have spread to other organs and tissues.
The types of radiation therapy most commonly used to treat cervical cancer are external beam radiation and brachytherapy. External beam radiation aims x-rays at the cancer from a machine outside the body. The treatment is similar to getting a regular x-ray, but the dose is much stronger. Brachytherapy, or internal radiation therapy, puts a source of radiation in or near the cancer. For cervical cancer, the most commonly used brachytherapy is intracavitary brachytherapy, in which a radiation source is placed in a device in the vagina and sometimes in the cervix.
Chemotherapy for cervical cancer
Chemotherapy uses anti-cancer drugs that are injected into a vein or given by mouth. They enter the bloodstream and can reach almost all areas of the body, making this treatment useful for killing cancer cells in most parts of the body.
Not all women with cervical cancer will need chemotherapy, but it is often recommended in combination with radiation therapy because it can help the radiation work better. It also may be recommended for cervical cancer that has spread or come back after treatment.
Targeted drug therapy for cervical cancer
This treatment uses medicines that target or are directed at proteins on cervical cancer cells that help them grow, spread, or live longer. Targeted drugs aim to destroy cancer cells or slow their growth.
Immunotherapy for cervical cancer
Immunotherapy uses specific medicines to boost a woman’s own immune system, helping it recognize and destroy cancer cells more effectively. Immunotherapy often works on specific proteins involved in the immune system to enhance the immune response. They have different and sometimes less severe side effects than chemotherapy.
Latest News from the Cancer Center
Loading items....
Information reviewed by Jill Alldredge, MD, in July 2025.