Contact UCHealth
Head and Neck Cancers
Shared Content Block:
News feed -- crop images to square
Contact Children's Hospital CO
Clinical Trials
Make a Gift
What Is Head and Neck Cancer?
Head and neck cancer is a general term for cancers that start in those regions of the body. Head and neck cancers include laryngeal (voice box) and hypopharyngeal (lower throat) cancer; oral cavity (tongue and gums) and oropharyngeal (tonsil and back of tongue) cancer; nasopharyngeal (upper throat behind the nose) cancer; nasal cavity and sinus cancer; and salivary gland cancer. Head and neck cancers typically begin in the squamous cells lining the mucosal surfaces inside the head and neck, including the nose, mouth, and throat.
According to the American Cancer Society, there are approximately 13,020 new cases and 3,910 deaths from laryngeal cancer and about 59,660 new cases and 12,770 deaths from oropharyngeal or oral cavity cancer each year.
Nasopharyngeal cancer (NPC), nasal cavity and paranasal sinus cancers, and salivary gland cancer are all very rare, with no set predictions on new cases and deaths provided.
Head and Neck Cancer Prognosis and Survival Rates
Head and neck cancer prognosis depends on the type of cancer and the stage at which it is diagnosed. Head and neck cancers account for around 4% of all cancers in the United States.
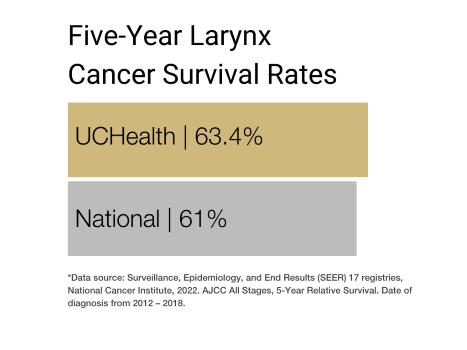
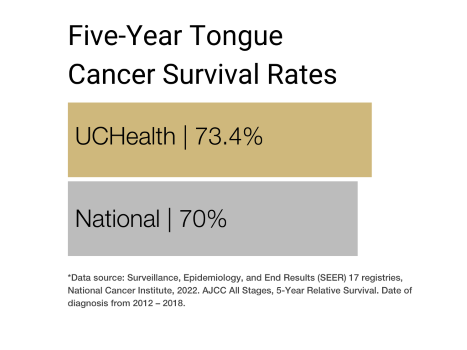
The five-year survival rate for head and neck cancer — the percentage of people who live at least five years after the disease is found —varies by the specific type of cancer. It ranges from 61% for nasopharyngeal, laryngeal and hypopharyngeal cancer to 76% for salivary gland cancer.
Why Come to CU Cancer Center for Head and Neck Cancer
As the only National Cancer Institute Designated Comprehensive Cancer Center in Colorado and one of only four in the Rocky Mountain region, the University of Colorado Cancer Center has doctors who provide cutting-edge, patient-centered head and neck cancer care and researchers focused on diagnostic and treatment innovations.
CU Cancer Center members have created Spanish-speaking navigation and care for head and neck cancer patients, called Esperanza en Español, or E3. Please call 720-598-2276 to speak with our patient navigator. Please leave a message if it is the weekend or after hours and we will return your call.
→ Learn more about how the E3 clinic started
The CU Cancer Center head and neck cancer program also has received a highly competitive Specialized Programs of Research Excellence (SPORE) grant from the National Cancer Institute. Designed to enable the rapid and efficient movement of basic scientific findings into clinical settings, as well as to determine the biological basis for observations made in individuals with cancer or in populations at risk for cancer, the SPORE grant directly impacts our cancer patient population in real time and enables access to and initiation of CU Cancer Center clinical trials that otherwise would not happen.
The CU Cancer Center has a multidisciplinary program for head and neck cancers. This is a great option for patients who are recently diagnosed, looking for a second opinion, or already in treatment. Our team will gather a group of surgical oncologists, medical oncologists, radiation oncologists, pathologists, dietitians, genetic counselors, and more to make sure each patient is getting the best care that is unique to his/her diagnosis.
There are numerous head and neck cancer clinical trials being conducted by CU Cancer Center members at any time. These trials offer patients options to traditional head and neck cancer treatment and can result in remission or increased life spans.
For more information on pediatric head and neck cancers, and to learn more about surgical treatment options with our clinical partner, visit the Pediatric Surgical Oncology Program and Solid Tumor team at Children’s Hospital Colorado.
Our clinical partnership with UCHealth has produced survival rates higher than the state average for all stages of sinuses and ear cancers, pharynx and other buccal cavity cancers and survival rates that are nearing the state average for all stages of larynx cancer and tonsil cancer.
Types of Head and Neck Cancer
Cancers of the head and neck are categorized according to the area in which they begin, typically the mouth, nose, or throat.
Laryngeal cancer starts in the larynx (voice box), while hypopharyngeal cancer starts in the hypopharynx, or lower throat. Almost all cancers in these areas start in the squamous cells, the thin, flat cells that make up the lining of the larynx and throat. Laryngeal cancer is much more common in men than women, and Black men are more likely to develop laryngeal cancer than white men.
Oral cavity cancer, also known as oral cancer, starts in the mouth, including the tongue and gums, while oropharyngeal cancer starts in the middle of the throat, just behind the oral cavity. Oral cavity and oropharyngeal cancer are more than twice as common in men as in women. They are slightly more common in white people than Black people. Oral cavity cancer is commonly related to use of tobacco and alcohol products. Oropharyngeal cancer can be related to tobacco and alcohol use as well, but it is more commonly caused by HPV (human papillomavirus).
Nasopharyngeal cancer starts in the nasopharynx, which is the upper part of the throat near the base of the skull, behind the nose. The most common type of nasopharyngeal cancer is nasopharyngeal carcinoma,
a cancer that starts in the cells lining the nasopharynx. Other types of cancers that can develop in the nasopharynx are lymphomas, which are cancers of immune system cells called lymphocytes; and adenocarcinomas and adenoid cystic carcinomas,
which can develop in small salivary glands within the nasopharynx.
Nasal cavity cancer starts in the opening behind the nose, and sinus cancer begins in the air-filled spaces that surround the bones around the nose. Types of nasal cavity and sinus cancer include:
- Squamous cell carcinomas, cancer of the flat cells that line the sinuses and the mucus-producing tissue (mucosa) that lines the nasal cavity and sinuses. Squamous cell carcinomas make up just over half of cancers of these areas.
- Salivary gland cancers formed in minor salivary glands.
- Sinonasal undifferentiated carcinomas (SNUC), which can form in mucosa cells.
- Melanoma, a type of cancer that starts in cells called melanocytes. Melanoma is typically found on sun-exposed areas of the skin, but it also can form on the lining of the nasal cavity and sinuses.
- Esthesioneuroblastoma, also known as olfactory neuroblastoma, a cancer that starts in the olfactory nerve. It typically starts in the roof of the nasal cavity.
- Lymphomas, cancers that form in immune system cells called lymphocytes.
- Sarcoma, a cancer of muscle, bone, cartilage, and fibrous cells that can form anywhere in the body.
Salivary gland cancers are rare cancers arising from one of the glands that makes saliva. The parotid gland is the most frequent site of salivary gland tumors, but they can also originate in the submandibular gland, sublingual gland, and other minor salivary glands throughout the head and neck mucosa. Different types of salivary gland cancers include:
- Adenoid cystic carcinoma
- Mucoepidermoid carcinoma
- Salivary duct carcinoma
- Carcinoma ex-pleomorphic adenoma
- Squamous cell carcinoma
- Acinic cell carcinoma
- Epithelial-myoepithelial carcinoma
- Polymorphous low-grade adencarcinoma
- Malignant mixed carcinoma
- Anaplastic or undifferentiated carcinoma
Risk Factors for Head and Neck Cancer
Head and neck cancer has multiple risk factors: behaviors or conditions that increase a person’s chances of getting a disease such as cancer. Smoking is a common risk factor among all head and neck cancers. Heavy to moderate alcohol use also
is a common risk factor; people who use both tobacco and alcohol are at highest risk. Human papillomavirus (HPV) infection is an increasingly prevalent risk factor and currently is the cause of the majority of oropharynx
cancers in North America.
Other risk factors for head and neck cancer include:
- Epstein-Barr virus infection (most often found in nasopharynx cancers).
- Use of oral tobacco products like snuff and chewing tobacco.
- Betel nut chewing.
- Immunodeficiency (impaired immune system) from chronic infections (like HIV and hepatitis B and C), transplants, hematologic malignancies (including leukemias and lymphomas), and long-term use of medications (including steroids and other immune suppressing medications).
- Excess body weight.
- Poor nutrition.
- Workplace exposure to asbestos, wood dust, paint fumes, and other chemicals.
- Genetic syndromes including Fanconi anemia and dyskeratosis congenita.
- Gender: Men are two to three times more likely to develop head and neck cancer.
- Age: Because they often take years to develop, head and neck cancers are most commonly found in those 50 and older.
- Exposure to sunlight.
- Family history of head and neck cancer.
Symptoms of Head and Neck Cancer
Head and neck cancers can usually be treated successfully if they are diagnosed before the cancer has spread to distant parts of the body. Patients with early-stage head and neck cancer may not experience symptoms, but those with later stages of the disease may.
Symptoms of head and neck cancer include:
- Hoarseness or other changes in the voice.
- A persistent sore throat.
- Painful swallowing or trouble swallowing.
- Trouble breathing.
- Ear pain or trouble hearing.
- Unexplained weight loss.
- Frequent coughing.
- Headaches.
- A lump or mass in the nose, mouth, neck, or throat.
- A sore in the mouth or on the lip that does not heal.
- Pain in the mouth.
- A white or red patch on the tongue, tonsil, gums, or lining of the mouth.
- Bad breath that is not due to hygiene.
- Frequent nosebleeds.
Screening for Head and Neck Cancer
Screening is used to look for cancer before a person shows any symptoms of the disease. There are no standard screenings for head and neck cancers, but oral and oropharyngeal cancers and pre-cancers often are discovered during routine oral exams by dentists or doctors. Those who use tobacco and/or alcohol are encouraged to look at their mouth in a mirror every month to look for white patches, sores, or lumps, which could be signs of cancer.
Diagnosing Head and Neck Cancer
Based on a patient’s symptoms and after an initial physical examination, a doctor may order certain tests to determine whether the patient has a head and neck cancer. Though testing procedures can vary based on the type of head and neck cancer the doctor is looking for, common screenings for head and neck cancer include:
Indirect pharyngoscopy and laryngoscopy: Doctors place small mirrors at the back of the mouth to examine the throat, tongue, and larynx.
Endoscopy: This procedure uses a flexible, fiber-optic scope, inserted through the nose or mouth, to take a closer look at parts of the throat, larynx, nose, and mouth.
Magnetic resonance imaging (MRI): An MRI uses radio waves and magnetic fields to produce detailed images of the body. In some situations, the doctor may order an MRI scan of the head and neck to get a more detailed picture.
Computed tomography (CT or CAT) scan: A CT scan uses X-rays to take detailed images of the body and can help identify several types of tumors. A CT scan can provide detailed information about the size, shape, and location of tumors in the head and neck and see if a tumor is growing into nearby tissues, lymph nodes, or organs.
Positron emission tomography (PET) scan: A slightly radioactive form of sugar is injected into the blood, where it is taken in by cells in the body. Since cancer cells grow faster than normal cells, they take in larger amounts of the sugar. Doctors use PET scans to look for possible areas of cancer spread, and to determine if suspicious areas seen on other imaging tests are cancer or not.
Biopsy: During a biopsy, a doctor extracts a sample (or multiple samples) of tissue from the suspected tumor site. These are sent to a laboratory for analysis by a pathologist to determine whether the cells in the sample are cancerous. There are different kinds of biopsies, and the type of biopsy a patient receives is determined by several factors, including the size and location of the tumor, the number of tumors, and the type of cancer suspected.
Stages of Head and Neck Cancer
After diagnosing the presence of head and neck cancer, the doctor will identify the stage of the disease. The stage is determined by several factors, including where exactly the disease formed, how extensive it is, and whether and how much it has spread.
Many of the same tests used to diagnose head and neck cancer are also used to identify the stage, including X-rays, CT/CAT scans, MRI scans, and PET scans.
Doctors typically use the TNM system established by the American Joint Committee on Cancer AJCC to determine the stage of head and neck cancer. The TNM system assesses the size and extent of the tumor (T) and whether it has spread; the involvement of nearby lymph nodes (N); and the presence and extent of metastasis (M) to other areas of the body, including the lungs, liver, and bones.
Head and Neck Cancer Stages
After the TNM assessment, the doctor will assign an overall stage number from I to IV. These can be broken down further based on the size of the original tumor and the extent to which the cancer has spread. Staging is complicated and differs by primary cancer site and in oropharynx cancer whether or not it is related to the human papillomavirus (HPV), but in general, the lower the stage the better the prognosis and treatment options.
Stage I: The primary tumor is small (typically less than two centimeters across), and the cancer has not spread to deeper layers of tissue, nearby structures, lymph nodes, or distant sites.
Stage II: The tumor is larger (measures 2-4 centimeters across) but the cancer has not spread to deeper layers of tissue, nearby structures, lymph nodes, or distant sites.
Stage III: The tumor fits one of these criteria:
- It is larger than 4 centimeters across, and the cancer has not spread to deeper layers of tissue, nearby structures, lymph nodes, or distant sites.
- It is any size but has not spread to nearby structures or distant sites. However, cancer cells are detected in one lymph node, located on the same side of the neck or head as the primary tumor, and the lymph node is smaller than three centimeters across.
Stage IV: The tumor may have spread to nearby structures or lymph nodes and may have also metastasized to distant lymph nodes, structures, or bones.
Treatments for Head and Neck Cancer
The treatment for head and neck cancer is customized to each patient and depends on the size and location of the tumor(s), the stage at which the patient is diagnosed, and the patient’s general health. Head and neck cancer care teams may include multiple health care specialists, including primary care providers, ear, nose and throat (ENT) specialists, medical oncologists, and radiation oncologists, as well as nurse practitioners, physician assistants, nurses, psychologists, dieticians, social workers, and rehabilitation specialists. CU Cancer Center doctors offer specialized care for patients with head and neck cancer.
Treatments for head and neck cancer include surgery, radiation therapy, chemotherapy, immunotherapy, and targeted drug therapy. Patients may receive one or more of these treatments in combination. Some patients may also be eligible to participate in clinical trials — doctor-led research studies of new or experimental procedures or treatments.
Radiation Therapy for Head and Neck Cancer
Radiation therapy uses high-powered energy to kill cancer cells. A doctor who specializes in radiation therapy to treat cancer is a radiation oncologist. The most common type of radiation therapy used to treat head and neck cancer is external beam radiation. Common radiation therapy side effects can include fatigue, radiation dermatitis (skin irritation, redness, blistering), soreness in the mouth and mucosa, dry mouth, changes in taste, swelling, and tooth decay. Many of these, including tooth decay, can be prevented or managed with proper treatment from a dentist before and after treatment.
External-beam radiation therapy (EBRT) is the most common radiation treatment and uses a machine located outside the body to focus a beam of X-rays on the area with the cancer. The two most common types of EBRT for head and neck cancer used at our center are intensity-modulated radiation therapy (IMRT) and stereotactic body radiation therapy (SBRT).
IMRT: This type of radiation maximizes the radiation delivered to the planned target while minimizing the radiation to normal tissue by delivering smaller doses of radiation over longer lengths of time. It is the most commonly used method of radiation for head and neck cancer.
SBRT: This type of radiation gives larger doses of radiation in shorter periods of time. It is most frequently given for recurrent tumors, in palliative settings, or in clinical trials.
Chemotherapy for Head and Neck Cancer
Chemotherapy uses drugs to kill rapidly growing cancer cells. The doctors that specialize in choosing and administering chemotherapy medications are called medical oncologists. Drugs are either injected into a vein or taken orally. For some head and cancers, chemotherapy is administered during the same time period as radiation, in a process called chemoradiation. Chemotherapy or chemoradiation can be used before surgery to shrink a tumor, making it easier to treat; in place of surgery, if feasible to avoid organ damage or removal; or after surgery to kill any cancer cells left behind after the operation. Chemotherapy also may be administered for cancer that has metastasized — or spread — to areas beyond the head and neck.
There are many different chemotherapy medications used in head and neck cancer, the most common ones being cisplatin, carboplatin, docetaxel and paclitaxel. All the medications have different side effect profiles, but frequent side effects can include fatigue, nausea and vomiting, constipation or diarrhea, decreased appetite, decreased taste, drops in blood counts, hearing changes, and other complications your oncologist will discuss with you.
Immunotherapy for Head and Neck Cancer
Sometimes the body’s immune system does not attack cancer because cancer cells produce proteins that help them hide from immune system cells. Immunotherapy, also called biologic therapy, boosts the patient’s immune system to help it attack and destroy cancer cells. In head and neck cancer, an effective immunotherapy approach is the use of immune checkpoint inhibitors or checkpoint blockade therapies — drugs that target the body’s checkpoint proteins, helping restore the immune system’s natural defenses against cancer cells. Currently, immunotherapy is approved to use in recurrent or metastatic head and neck cancer as well as prior to surgery for some head and neck cancers. There are ongoing clinical trials studying it in other stages and settings.
Pembrolizumab (Keytruda), Nivolumab (Opdivo), and Toripalimab-tpzi (Loqtorzi) are immunotherapy drugs that target PD-1, a protein on T cells in the immune system. Normally, PD-1 prevents T cells from attacking other cells. By blocking PD-1, the immunotherapy drugs boost the immune response to cancer cells.
Targeted Drug Therapy for Head and Neck Cancer
Targeted therapy focuses on the specific genes, proteins, or tissue environments that contribute to cancer, limiting damage to non-cancerous cells and tissues.
The most common targeted drug therapies for head and neck cancer include:
EGFR-targeted drugs: Epidermal growth factor receptor (EGFR) is a protein that helps cancer cells grow. Drugs like Cetuximab (Erbitux) that inhibit EGFR are used to treat some cancers of the head and neck. Cetuximab may be used to treat cancers that have spread or have come back after treatment. It may be combined with radiation and/or chemotherapy drugs.
Other targeted drugs continue to be evaluated and studied in laboratory and clinical trials.
Surgery for Head and Neck Cancer
Several surgeries exist for head and neck cancer, depending on where the tumor is located. Some of the most common include:
Cordectomy: In this surgery, part or all of the vocal cords are removed. A cordectomy may be used to treat laryngeal cancer that is very small or located just on the surface tissues. A cordectomy may result in changes in speech.
Flexible robotic surgery: This minimally invasive treatment option allows surgeons to access hard-to-reach areas of the throat and mouth using a thin, flexible scope.
Free flaps: Using a process called microvascular surgery, in which small blood vessels are sewn together under a microscope, the throat can be reconstructed using tissues from other parts of the body, such as the arm or leg muscle and skin.
Glossectomy: This surgery removes part or all of the tongue.
Laryngectomy: This surgery removes part or all of the larynx.
Lymph node removal: Cancer of the head and neck can spread to lymph nodes in the neck. If a doctor thinks this has happened, they may recommend removing the lymph nodes. The operation — called a neck dissection — often is performed at the same time as surgery to remove the primary tumor. The exact amount of tissue removed depends on the stage and location of the cancer.
Myocutaneous flaps: In this operation, the throat is reconstructed using muscle and skin from a nearby area.
Partial laryngectomy: For some small laryngeal cancers, surgeons are able to remove just the affected portion of the larynx, leaving the rest of the voice box intact. A partial laryngectomy can involve removing either the portion of the larynx above the vocal cords (supraglottic laryngectomy), or just one of the two vocal cords (hemilaryngectomy).
Pharyngectomy: This surgery removes part or all of the throat.
Tonsillectomy: This surgery removes one or both of the tonsils.
Total laryngectomy: This procedure removes the entire voice box, followed by a process called a tracheostomy, where an opening is created in the windpipe so a tube can be inserted for breathing.
Transoral robotic surgery (TORS): This surgery is a less invasive way to remove smaller oropharynx tumors.
Vocal cord stripping: In this surgery, a surgeon uses a long instrument to remove the outer layers of tissue on the vocal cords. It is often used to take a biopsy sample or to treat cancer that is confined to the vocal cords. Vocal cord stripping rarely impacts speech.
The University of Colorado (CU) Cancer Center partners with UCHealth, Children’s Hospital Colorado, and Rocky Mountain Regional VA to provide clinical care. Please make an appointment with one of our clinical partners to be seen by a CU Cancer Center doctor.
UCHealth Cancer Care - Anschutz Medical Campus
1665 Aurora Court Anschutz Cancer Pavilion
Aurora, CO 80045
720-848-0300
UCHealth Cherry Creek Medical Center
100 Cook Street
Denver, CO 80206
720-848-0000
UCHealth Cancer Center - Highlands Ranch
1500 Park Central Drive
Highlands Ranch, CO 80129
720-516-1100
Children's Hospital Colorado:
13123 East 16th Avenue
Aurora, CO 80045
720-777-6740
Rocky Mountain Regional VA Medical Center:
1700 North Wheeling Street
Aurora, CO 80045-7211
303-399-8020
Latest in Head and Neck Cancer from the Cancer Center
Loading items....
Information reviewed by Jessica McDermott, MD, in September 2025.