Contact UCHealth
Lung Cancer
Clinical Trials
Make a Gift
What Is Lung Cancer?
The lungs are two spongy organs in the chest that take in oxygen when you inhale and expel carbon dioxide when you exhale. Air enters through the mouth, nose, and trachea then divides into tubes called bronchi. Like the roots of a tree, the bronchi split off into smaller branches called bronchioles, and at the end of the bronchioles are tiny air sacs called alveoli that absorb oxygen into the bloodstream when you inhale and remove carbon dioxide when you exhale. The right lung is made up of three lobes and the left lung is made of two lobes to make more room for the heart. Lung cancer most commonly starts in the cells lining the bronchi, bronchioles, and alveoli.
According to the American Cancer Society, in the United States, more than 234,580 new cases of lung cancer are diagnosed and there are an estimated 125,070 deaths from the disease each year. Lung cancer is most commonly diagnosed among those 65 or older, with a very small amount of people diagnosed younger than 45. Lung cancer is the leading cause of cancer death among men and women, making up about one in five of all cancer deaths.
The chance a man will develop lung cancer is about one in 16, and for women, the risk is about one in 17. Black men are 12% more likely to develop cancer than white men, but the rate of lung cancer in Black women is 16% lower than in white women.
In Colorado, there are an estimated 2,660 new cases and 1,290 deaths from lung and bronchus cancer each year.
Why Come to CU Cancer Center for Lung Cancer
The CU Cancer Center is home to one of the world’s best known lung cancer teams. The team has led many different breakthroughs in how to treat cancers that affect the lungs — both for non-small cell lung cancer and small cell lung cancer and other rare cancers of the chest, such as mesothelioma or thymic cancer.
The CU Cancer Center is the only National Cancer Institute-Designated Comprehensive Cancer in Colorado. Our doctors provide top-notch, multidisciplinary, patient-centered care, and we offer treatment options not available at most other medical centers in the country. Our lung care team has a broad catchment area, providing care from coast to coast. Importantly, our team specializes in thoracic cancers, allowing us to keep at the very cutting edge of research and the best possible treatment decisions for our patients.
Our doctors are the only physicians in a 500-mile radius who are part of the National Comprehensive Cancer Network (NCCN) advisory panel. The NCCN establishes treatment guidelines that doctors all across the United States use as a reference. The lung cancer care team serves on the NCCN lung cancer screening, surviving, and smoking cessation panels.
The Thoracic Oncology Research Initiative (TORI), a program advancing lung cancer research at the University of Colorado Cancer Center, is comprised of a multidisciplinary team of investigators from multiple departments and centers across the University of Colorado Anschutz Medical Campus. TORI’s multidisciplinary team includes basic, translational and clinical scientists with expertise in molecular biology, cellular biology, biochemistry, medicinal chemistry, radiation biology, bio-informatics, health disparities, lung cancer prevention and early detection, and pre-clinical studies. TORI is committed to fostering collaborations between these disciplines and departments with the goal of acquiring funding to initiate new programs and innovative clinical trials within the CU Cancer Center and across the institution. There are over 160 lung cancer clinical trials, currently being offered by CU Cancer Center members, giving patients many different treatment options.
The Lung Multidisciplinary Clinic at the CU Cancer Center brings together a team of expert thoracic surgeons, medical oncologists, pathologists, radiologists, and more to focus on problems affecting the lungs. Together, the team analyzes a patient’s diagnosis and recommends a specific treatment plan for the individual by the end of the visit. All of our providers subspecialize in cancers of the lung and chest, utilizing the newest research and treatments of lung and related cancers. Contact the Thoracic Multidisciplinary Clinic at 720-848-0147.
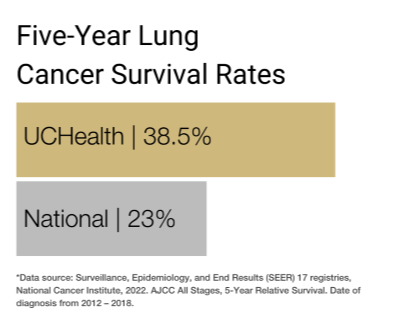
Our clinical partnership with UCHealth has produced survival rates higher than the state average for all stages of lung cancer.
Types of Lung Cancer
There are two broad types of lung cancers, non-small cell lung cancer (NSCLC) and small-cell lung cancer (SCLC). About 13% of all lung cancers are small-cell lung cancer and 84% are non-small cell lung cancer.
The most common subtypes of non-small cell lung cancer include:
Adenocarcinomas start in the cells that secrete mucus. They occur mainly in individuals who smoke or have a history of smoking but are also the most common type among individuals who do not have a history of smoking. Adenocarcinomas are more common in women than in men and are more commonly diagnosed in younger people than other types of lung cancers.
Squamous cell carcinomas start in the squamous cells, flat cells that line the inside of the bronchi and bronchioles. Squamous cell carcinomas are often linked to smoking and are often found near the bronchus.
Large cell carcinomas appear in any part of the lung and grow and spread quickly, making them difficult to treat.
Small-cell lung cancer grows and spreads faster than non-small cell lung cancer. About 70% of people with small-cell lung cancer are diagnosed with cancer that has already spread. This type of lung cancer responds well to chemotherapy and radiation but is reoccurring in most cases.
Causes of Lung Cancer
Smoking tobacco is a predominant cause of most lung cancers. Importantly, not all people who get lung cancer have a history of smoking or are exposed to secondhand smoke. Exposure to radon, air pollution, asbestos, and diesel exhaust, among other chemicals, can cause lung cancers in individuals who have not smoked.
→ Hear from two non-smoking lung cancer patients
DNA changes or mutations that occur within healthy lung cells can lead to abnormal growth and cancer. Cells contain DNA that tells the cell what to do. When a cell’s DNA is damaged, cells continue to grow and divide where they aren’t needed by the body. This buildup of cells becomes a tumor.
Risk Factors for Lung Cancer
There are several factors that might increase the chance of developing lung cancer. These risk factors include:
Smoking: By far the leading risk factor for lung cancer, smoking accounts for upward of 80% of lung cancer deaths. Small-cell lung cancer is very rarely diagnosed in people who have never smoked.
Secondhand smoke: It is believed that more than 7,000 deaths from lung cancer are caused by secondhand smoke each year.
Radon: This naturally occurring radioactive gas is a result of uranium breaking down in soil and rocks. It is odorless and tasteless and the second leading cause of lung cancer in the United States. It is the leading cause among non-smokers.
Asbestos: This naturally occurring mineral is commonly used in mines, mills, textile plants, and shipyards. People who work with asbestos are more likely to die from lung cancer.
Previous radiation: People who receive radiation therapy on or near their chest for other cancers have a higher risk for lung cancer. This does not include women who have radiation therapy to the breast.
Symptoms of Lung Cancer
Symptoms of most lung cancers do not appear until the cancers have spread.
Lung cancer can cause a number of symptoms or complications, such as:
Persistent cough: Many lung cancer patients experience a cough that does not go away or gets worse. This cough can also cause bleeding in the airway and lead to coughing up blood.
Shortness of breath: Increase shortness of breath is experienced by patients as the cancer grows and blocks the airways. Lung cancer can also cause fluid buildup in the space that surrounds the lungs (pleural effusion).
Pain: Advanced lung cancer that spreads to the lining of the lung can cause the patient chest pain when breathing, coughing, or laughing. In cases where the cancer has spread to another area of the body, the patient may experience bone pain, headaches, weakness, and/or swelling of lymph nodes.
Infections: Persistent bronchitis and pneumonia can be indicators of cancer developing in the lungs.
Jaundice: Also known as yellowing of the skin or eyes.
Diagnosing Lung Cancer
Some lung cancers can be found by screening, although the current criteria for screening are primarily based on smoking-related risk factors and age. Some are found incidentally when having scans or x-rays done for other reasons. However, most lung cancers are discovered because the patient is experiencing symptoms. Exams, tests, and procedures to diagnose lung cancer include:
Imaging tests: To help find suspicious looking areas of the lungs or reveal abnormal masses or nodules, imaging tests like a chest x-ray, CT scan, MRI scan, PET scan, or bone scan may be ordered.
- A chest X-ray is most commonly the first test a doctor will do to look at the lungs.
- A CT scan uses x-rays to take detailed images of the body and can help identify lung cancer tumors. A CT scan can provide detailed information about the size, shape, and location of tumors in the lungs. A CT scan may also reveal lung cancer that has spread to the adrenal glands, liver, brain, and other organs.
- MRI scans use magnetic pulses to take images of the soft tissues of the body. MRIs can be used to look for possible spread of lung cancer to the brain or spinal cord.
- A PET scan is a test that uses a radioactive form of sugar injected into the blood that collects around cancer cells. A PET/CT is a special machine that combines both tests to allow doctors to compare areas of high radioactivity on the PET scan with a detailed image on the CT scan.
Sputum cytology: For patients with a persistent cough who are producing sputum, mucus coughed up from the lungs, a sample of the sputum can be collected and looked at in a lab to see if cancer cells are present. To best conduct this test, patients should collect samples early in the morning three days in a row. Cancers in the major airways, such as squamous cell lung cancers, are commonly found from a sputum cytology.
Thoracentesis: Patients experiencing pleural effusion, fluid buildup in the lungs, can have some of the fluid drained by a doctor and tested in a lab for cancer cells. This test is conducted by inserting a long hollow needle into the pleura to drain the fluid. After a thoracentesis the fluid can continue to build up causing trouble breathing and pain, in these cases the procedure may be repeated.
Needle biopsy: During this procedure, a hollow needle is inserted into a portion of the lung to get a small sample from the suspicious area or mass. In some cases, this small sample may not provide enough tissue to make a firm diagnosis and more tests may be ordered. Two additional needle biopsies include the fine needle aspiration biopsy and the core biopsy.
- Fine needle aspiration (FNA) biopsy is a procedure where the doctor uses a syringe with a thin hollow needle to withdraw cells and small tissue samples.
- Transtracheal FNA or transbronchial FNA uses a needle passed through the wall of the trachea or bronchi to collect cells.
- Core biopsy is a procedure that uses a larger needle to remove one or more small cores of tissue from the lungs. This test is preferred over FNA biopsies.
Bronchoscopy: A procedure during which a scope is passed down the throat into the bronchi to look for tumors or blockages in the larger areas of the lungs. Biopsies may be taken during this procedure.
Endobronchial ultrasound: An ultrasound can be used to see the lymph nodes and other structures to help guide needles if biopsies need to be taken.
Endoscopic esophageal ultrasound: This test allows the doctor to look down into the esophagus and nearby lymph nodes which may have abnormal areas of lung cancer cell growth.
Mediastinoscopy: This procedure uses a scope inserted behind the sternum under general anesthetic to look at and take samples from the lymph nodes along the trachea and bronchial tubes.
Lung function tests: Pulmonary function tests (PFTs) are done after a lung cancer diagnosis to test how the lungs are working. In surgical cases, where part of the lung is removed, a pulmonary function test may be done before the surgery to determine how well the lungs are working beforehand. Some people with lung damage from smoking don’t have enough undamaged lung to allow for the removal of the part of the lung. These tests help surgeons determine if surgery is an option.
Blood tests: Blood tests are not commonly used to diagnose lung cancer; however, they can provide details on a patient’s health.
- A complete blood count (CBC) looks at the blood and records the numbers of types of blood cells, including red blood cells, white blood cells, and platelets. Lower levels of red blood cells mean the bone marrow is not functioning properly, elevated levels of white blood cells mean there is an infection the body is trying to fight off, and a low platelet count means the blood has low clotting factors.
- Blood chemistry tests can help identify abnormalities in some organs like the liver or kidneys.
Analysis of lung cancer cells in a lab help determine the lung cancer type. Results of these tests and procedures help determine the patient’s prognosis and guide treatment.
Stages of Lung Cancer
Once lung cancer has been diagnosed, tests and procedures will help determine the extent of cancer. The cancer’s stage guides which treatments are appropriate.
The most commonly used staging system for non-small cell lung cancer and small-cell lung cancer is from the American Joint Committee on Cancer. The TNM system assesses the size and extent of the tumor (T-tumor); whether the cancer has spread to nearby lymph nodes (N-node); and the presence and extent of metastasis (M-metastasis) to distant lymph nodes and organs like the brain, bones, or adrenal glands.
Lung cancer is staged based on the results of tests performed like physical exams, biopsies, and imaging tests.
Non-Small Cell Lung Cancer Stages
Occult cancer: Cancer cells are detected in sputum or other lung fluids but the cancer isn’t found with other tests so the location cannot be determined. It is not thought to have spread to nearby lymph nodes or distant sites.
Stage 0: Called carcinoma in situ, a tumor is found only in the top layer of cells lining the air passages of the lungs and has not invaded deeper into other lung tissues. The cancer has not spread to nearby lymph nodes or distant sites.
Stage 1: The cancer is located only in the lungs, is only in the top layers of tissue, and has not yet spread to deeper lung tissue, to the outside of the lungs, lymph nodes. or distant sites.
Stage 2: The cancer has penetrated the deeper tissue of the lungs, to the outside of the lungs, and has spread to nearby lymph nodes.
Stage 3: The cancer has been found in the lung and the lymph nodes in the center of the chest.
Stage 4: The cancer has spread to both lungs, to the lymph nodes, and distant parts of the body such as the liver, brain, or bones.
These stages can be further broken down based on the size of the original tumor and the extent to which the cancer has spread.
Small-Cell Lung Cancer Stages
For treatment purposes, small-cell lung cancer is categorized into two stages, limited stage and extensive stage.
Limited stage: The cancer is only on one side of the chest, confined to one lung, or may have also reached the lymph nodes on the same side of the chest. A patient with limited stage small-cell lung cancer may benefit from more aggressive treatments. Only 1 in 3 people with small-cell lung cancer have limited stage cancer when diagnosed.
Treatments for Non-Small Cell Lung Cancer
Treatment for lung cancer is tailored to each patient and is dependent on the stage of the cancer, where it is located, and other health concerns. Lung cancer care teams may include multiple health care specialists including thoracic surgeons, medical oncologists, pathologists, radiologists, and more.
Surgery for Non-Small Cell Lung Cancer
Surgery to remove the cancer is an option for some early-stage non-small cell lung cancers. In order to determine if a patient is a good candidate for surgery a surgeon will order a pulmonary function test to see if there is enough healthy lung tissue. They will also order tests to check the function of the heart and other organs.
Pneumonectomy is a surgery where the entire lung is removed because of a tumor located close to the center of the chest.
Lobectomy is the removal of one of the 5 lung lobes containing the cancer. This is the preferred type of operation for non-small cell lung cancer.
Segmentectomy is the removal of part of a lung lobe.
Sleeve resection is an operation that may treat cancers located in the larger airways of the lungs. If the cancer is located in the bronchi or bronchioles, a portion in the middle of the tube is resected and then the two ends can be reconnected.
Video-assisted thoracic surgery (VATS), also known as a thoracoscopy, this procedure is more frequently being used to treat early-stage lung cancers. The instruments are inserted through smaller incisions which allows for a shorter hospital stay and fewer complications. During this procedure, the part of the lung that contains the tumor or the entire lobe is removed.
Robotic-assisted thoracic surgery (RATS) is a thoracoscopy that is done using a robotic system. Similar to video-assisted thoracic surgery, robotically-assisted thoracic surgery uses smaller incisions and reduces hospital stay and potential complications.
Radiation Therapy for Non-Small Cell Lung Cancer
Radiation is a treatment that uses high-energy rays or particles that destroy cancer cells and shrink tumors. Radiation might be used as the main treatment for nonresectable tumors because of their size or location. Radiation may sometimes be used after surgery to kill any small cancer cells left behind or before surgery to help shrink tumors. Radiation therapy is often combined with chemotherapy as a treatment option.
External beam radiation therapy is the most common type of radiation therapy used to treat non-small cell lung cancer. There are three newer external beam radiation therapy techniques that have been shown to help treat lung cancers. These include:
- Stereotactic body radiation therapy (SBRT) is used to treat early-stage lung cancer when surgery isn’t an option. This treatment uses focused beams of high-dose radiation given in 1 to 5 treatments.
- Three-dimensional conformal radiation therapy (3D-CRT) uses computers to map the tumor and then the beams are aimed at the tumor from several directions.
- Intensity modulated radiation therapy (IMRT) is a 3D therapy where the strength of the beams can be adjusted.
Chemotherapy for Non-Small Cell Lung Cancer
Chemotherapy is a treatment that uses drugs that travel through the bloodstream to reach cancer cells in most parts of the body.
Neoadjuvant chemotherapy, sometimes paired with radiation therapy, is given before an operation to help reduce the cancer’s size to make it easier to remove with surgery.
Adjuvant chemotherapy is given after surgery, sometimes with radiation therapy, to kill any cancer cells that may have been left behind. Adjuvant chemotherapy helps lower the risk of cancer recurrence.
For locally advanced non-small cell lung cancer, chemotherapy along with radiation is given as the main treatment when surgery is not an option. For some cancers, this combination of chemotherapy and radiation can still be a cure.
For metastatic non-small cell lung cancer, chemotherapy is given when the cancer has spread outside the lung to other areas such as the bones, liver, and adrenal glands.
Targeted Drug Therapy for Non-Small Cell Lung Cancer
Targeted drugs are used to target the changes in cells that cause cancer. Often these are pills and are based on finding specific mutations or other genetic changes in the lung cancer.
Immunotherapy for Non-Small Cell Lung Cancer
Immunotherapy uses drugs to train the immune system to enhance the body’s ability to fight cancer. One of the most important characteristics of the immune system is its ability to recognize and avoid attacking the body's normal cells. To do this, it uses “checkpoint” proteins on immune cells. Cancer cells sometimes use these checkpoints to keep the immune system from attacking them. Drugs that target these checkpoints — called checkpoint inhibitors — can correct this.
PD-1 inhibitor is a checkpoint protein on T cells which, when attached to a PD-L1, another protein, tells the T cell to ignore the other cell.
Atezolizumab (Tecentriq) targets the PD-L1 protein by blocking the protein to boost the immune response against cancer cells.
Durvalumab (Imfinzi) targets PD-L1 protein. The goal of this drug is to keep the cancer from progressing.
CTLA-4 inhibitor Ipilimumab (Yervoy) is a drug that boosts the immune response by blocking CTLA-4, a protein on T cells that helps keep them in check.
Treatments for Small-Cell Lung Cancer
Surgery for Small-Cell Lung Cancer
Surgery is rarely used as the main treatment for small-cell lung cancer. Fewer than 1 in 20 patients have early-stage cancers that are treatable with surgery. When surgery is an option there are four options, pneumonectomy, lobectomy, segmentectomy, and sleeve resection.
Chemotherapy for Small-Cell Lung Cancer
Chemotherapy uses drugs to kill the cancerous cells, it can be given through your arm (IV) or by a pill. Chemo is the main treatment for small-cell lung cancer because when most patients are diagnosed, it has already spread and other treatments like surgery and radiation would not be able to reach all of the areas of cancer. Patients with limited stage small-cell lung cancer are often given radiation therapy with chemotherapy. Patients with extensive stage small-cell lung cancer are given chemo sometimes with immunotherapy.
Radiation Therapy for Small-Cell Lung Cancer
Radiation therapy uses high-energy beams and protons to kill cancerous cells. In some cases, for tumors and lymph nodes in the chest, concurrent chemoradiation, radiation in combination with chemotherapy, can be used. Radiation can also be used after chemo for patients with extensive stage lung cancer. Prophylactic cranial irradiation is used to lower the chances of cancer spreading to the brain and can also help patients with extensive stage lung cancer.
External beam radiation therapy is the most common type of radiation therapy used to treat small-cell lung cancer, same as non-small cell lung cancer. The three types of external beam radiation therapies available are, stereotactic body radiation, three-dimensional conformal radiation therapy, and intensity modulated radiation therapy.
Immunotherapy for Small-Cell Lung Cancer
Immunotherapy is the use of drugs to boost the body’s immune system to fight cancer cells. These drugs utilize “checkpoint” proteins to recognize cancer cells and attack them. Commonly used checkpoint inhibitors for small-cell lung cancer include Pembrolizumab (Keytruda) and Atezolizumab (Tecentriq), which both target proteins, PD-1 and PD-L1, to boost the immune response against cancer cells.
Our Thoracic Multidisciplinary Team
Latest in Lung Cancer from the Cancer Center
Loading items....
Information reviewed by Jamie, Studts, PhD, January 2023.