Contact UCHealth
Ovarian Cancer
Clinical Trials
Make a Gift
What Is Ovarian Cancer?
Ovarian cancer broadly refers to cancer that starts in the ovaries, fallopian tubes, or, less commonly, the lining of the abdominal cavity, called the peritoneum. The ovaries are glands in females that produce eggs for reproduction. During reproduction, eggs travel from the ovaries through the fallopian tubes and into the uterus, where a fertilized egg can settle to develop into a fetus. The ovaries are also the primary source of the female hormones estrogen and progesterone. Most women have two ovaries, one on either side of the uterus.
Often, ovarian cancer can go undetected until it starts to spread beyond the ovary and further into the abdomen and pelvis. At that point, the cancer is referred to as late-stage ovarian cancer and is generally more difficult to treat. Early-stage ovarian cancer describes disease that is confined to the ovary and is typically easier to treat and often has a better prognosis.
According to the American Cancer Society, there are approximately 19,680 new cases and 12,740 deaths from ovarian cancer each year in the United States. In Colorado, it is estimated that 290 people will be diagnosed with ovarian cancer and 200 will die from the disease.
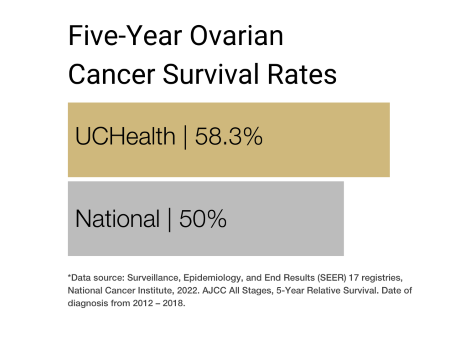
Ovarian Cancer Prognosis and Survival Rates
Ovarian cancer is the fifth most common cause of cancer-related deaths in women in the U.S. The risk of a woman getting ovarian cancer during her lifetime is around one in 87, while the lifetime odds of a woman dying from ovarian cancer are around one in 130.
Ovarian cancer develops primarily in older women. More than half of women diagnosed with ovarian cancer are 63 or older. Ovarian cancer is more common in white women than Hispanic, Asian/Pacific-Islander, African American, or American Indian/Alaska Native women.
The rates of ovarian cancer diagnoses have been falling slowly over the past two decades.
The five-year survival rate for ovarian cancer — the percentage of people who live at least five years after the disease is found —varies by the specific type of ovarian cancer and the stage at which it is discovered. It ranges from 31% for invasive epithelial ovarian cancer that has spread to distant parts of the body, such as the liver or lungs, to 97% for ovarian stromal tumors and germ cell tumors of the ovary that are discovered and treated before they can spread.
Of all ovarian cancers, 90% to 95% fall within the category of “epithelial” ovarian carcinomas, which include the serous, mucinous, endometrioid, and clear cell subtypes, as well as borderline tumors of low malignant potential. The remaining 5% to 10% are germ cell and sex cord stromal tumors, which arise from the specialized gonadal stroma surrounding the oocytes, such as the granulosa, theca, Sertoli, and Leydig cells, and are more commonly seen in younger women. Of the epithelial carcinomas, 75% are serous.
Until recently, fallopian tube and peritoneal carcinomas were thought to be phenotypically related, but clinically distinct from ovarian cancer and were considered relatively rare. However, recent data suggest that most epithelial ovarian cancers originate in the fallopian tube, and given their similar behavior, these three are often treated as a single entity.
Why Come to CU Cancer Center for Ovarian Cancer
As the only National Cancer Institute Designated Comprehensive Cancer Center in Colorado and one of only four in the Rocky Mountain region, the University of Colorado Cancer Center has doctors who provide cutting-edge, patient-centered ovarian cancer care, as well as researchers who are dedicated to finding cutting-edge diagnostic and treatment modalities.
The Women’s Cancer Developmental Therapeutics Program (WCDTP) at the CU Cancer Center seeks to increase the development of novel cancer therapies in ovarian cancer and other gynecologic cancers with the goal of decreasing cancer-related morbidity and mortality for patients. Additionally, the WCTD seeks to increase access to phase I and II clinical trials of novel cancer therapies for patients with gynecologic and breast cancers.
There are numerous clinical trials ongoing at the CU Cancer Center at any one time, including trials that enroll ovarian cancer patients. These trials offer patients other options besides traditional ovarian cancer treatment.
→ CU Researchers Come Together to Better Understand Ovarian Cancer Tumors and Treatment Outcomes
For more information on pediatric ovarian cancer, and to learn more about the care options with our clinical partner, visit the Pediatric Surgical Oncology Program and Solid Tumor team at Children’s Hospital Colorado.
Types of Ovarian Cancer
Different types of cells in the ovaries can become cancerous, and the type of cell affected determines the type of ovarian cancer. Ovarian cancer type can be determined by looking at the cells under a microscope. Doctors use this information to understand and make predictions about the anticipated rate of growth and pattern of tumor spread, and to determine which treatments may work best.
There are three main types of ovarian cancer, named for the cells in which the tumors originate.
- Epithelial tumors start in the cells covering the outer surface of the ovary. Most ovarian tumors are epithelial cell tumors.
- Germ cell tumors start in the cells that produce eggs. Less than 2% of ovarian tumors are germ cell tumors.
- Stromal tumors start in the structural connective tissue cells that hold the ovary together and produce the hormones estrogen and progesterone. Stromal tumors are rare and occur mostly in younger women.
Risk Factors for Ovarian Cancer
Ovarian cancer has multiple risk factors, or behaviors or conditions that increase a person’s chances of getting the disease. Risk factors for ovarian cancer include:
- Age: Ovarian cancer can occur at any age, but it is most common in women ages 50 to 60.
- Inherited gene mutations: A small number of ovarian cancers are caused by gene mutations, which are inherited from your parents. Genes known to increase ovarian cancer risk are breast cancer gene 1 (BRCA1) and breast cancer gene 2 (BRCA2). These genes also increase the risk of breast cancer. Other gene mutations, including mutations associated with Lynch syndrome, can also increase the risk of ovarian cancer.
- Family history of ovarian cancer: Women with two or more close relatives with a history of ovarian cancer are at increased risk for the disease.
- Estrogen hormone replacement therapy: This is especially true for those with long-term use, or those who have received hormonal therapy at large doses.
- Age when menstruation started and ended: Women who started menstruating at an early age or started menopause at a later age — or both — may be at increased risk for ovarian cancer.
Symptoms of Ovarian Cancer
Ovarian cancers can usually be treated successfully if they are diagnosed before the cancer has spread to other parts of the body. Patients with early-stage ovarian cancer may not experience symptoms, but those with later stages of the disease often do.
Symptoms of ovarian cancer include:
- Abdominal swelling or bloating.
- Feeling full quickly when eating or trouble eating.
- Weight loss.
- Pain in the stomach or pelvic area.
- Constipation or other changes in bowel habits.
- A frequent or urgent need to urinate.
Screening for Ovarian Cancer
Screening is used to look for cancer before a person shows any symptoms of the disease. No screening regimen has been found to be effective for ovarian cancer, but it can sometimes be detected during a regular pelvic exam. If a patient has symptoms, doctors can perform tests that help detect the presence of tumors.
→ Donors Supporting the CU Cancer Center are Building Towards Early Detection of Ovarian Cancer
Diagnosing Ovarian Cancer
Based on a patient’s symptoms and after an initial physical examination, a doctor may order certain tests to determine whether a patient has ovarian cancer. Though testing procedures can vary based on the type of ovarian cancer the doctor is looking for, common tests for ovarian cancer include:
Laparoscopy: In this procedure, a doctor inserts a thin, tubular camera through a small incision in the abdomen to view the ovaries and other pelvic organs and tissues. Once inside the abdomen, the camera transmits images to a video monitor, which allows the surgeon to perform biopsies and other necessary procedures.
Colonoscopy: Used to examine the inside of the large intestine (colon), colonoscopies are conducted with a small, flexible, lighted tube that has a small video camera attached to the end. The tube is inserted through the anus and into the rectum and colon, usually under light sedation or anesthesia. Any abnormal areas can be biopsied during the screening.
Imaging tests: Different imaging procedures can provide information about the extent of ovarian cancer in the body and reveal the presence of infections or other problems. The following imaging tests may be used to help formulate a blood cancer diagnosis:
- Ultrasounds
- Computed tomography (CT) scans
- Magnetic resonance imaging (MRI) scans
- Barium enema X-ray
Biopsy: During a biopsy, a doctor extracts a sample (or multiple samples) of tissue from a suspected tumor site. These are sent to a laboratory for analysis by a pathologist to determine whether the cells in the sample are cancerous or precancerous. There are different kinds of biopsies, and the type of biopsy a patient has is determined by several factors, including the size and location of the tumor, the number of tumors, and the type of cancer suspected. Importantly, not all ovarian cancers can be biopsied before surgery, as this can risk causing tumor spread.
Stages of Ovarian Cancer
After diagnosing the presence of ovarian cancer, the doctor will determine what steps are necessary to identify the stage of the disease and what treatment is necessary based on that information. Disease stage is determined by several factors, including where exactly the disease formed, how extensive it is, and whether and how much it has spread. Staging for ovarian cancer can be achieved by taking tissue samples for diagnosis and, more often, by doing surgery to remove affected areas.
Doctors typically use the International Federation of Gynecology and Obstetrics’ FIGO system and the American Joint Committee on Cancer’s TNM system to determine the stage of ovarian cancer. The TNM system assesses the size and extent of the tumor (T); the involvement of nearby lymph nodes (N); and the presence and extent of spread, or metastasis (M), to other areas of the body, including the lungs, liver, and bones.
After TNM assessment, the doctor will assign an overall stage number from I to IV. These can be broken down further based on the size of the original tumor and the extent to which the cancer has spread. In general, the lower the stage, the better the prognosis and treatment options.
Stage I: The cancer is located only in one or both ovaries or fallopian tubes and has not spread to nearby lymph nodes, or to distant sites.
Stage IA: The cancer is in one ovary and/or fallopian tube, and the tumor is confined to the inside of the ovary or tube. There is no cancer on the outer surfaces, and no cancer cells are found in the peritoneal fluid (ascites), or washings from the abdomen and pelvis. The disease has not spread to nearby lymph nodes or distant sites.
Stage IB: The cancer is in both ovaries, or both fallopian tubes, but not on their outer surfaces. No cancer cells are found in the peritoneal fluid (ascites), or washings from the abdomen and pelvis. It has not spread to nearby lymph nodes or distant sites.
Stage IC: The cancer is in one or both ovaries or fallopian tubes, and any of the following are present:
- Stage IC1: The tissue (capsule) surrounding the tumor tore or ruptured during surgery, potentially allowing cancer cells to leak into the abdomen and pelvis (also known as surgical spill).
- Stage IC2: Cancer is on the outer surface of at least one of the ovaries or fallopian tubes, or the capsule (tissue surrounding the tumor) ruptured before surgery, allowing cancer cells to spill into the abdomen and pelvis.
- Stage IC3: Cancer cells are found in the fluid (ascites) or washings from the abdomen and pelvis.
In all IC cases, the cancer has not spread to nearby lymph nodes or distant sites.
Stage II: The cancer involves one or both ovaries or fallopian tubes and has spread to other organs within the pelvis (such as the uterus, bladder, the sigmoid colon, or the rectum), or there is primary peritoneal cancer. It has not spread to nearby lymph nodes or distant sites.
Stage IIA: The cancer has spread to or invaded the uterus or the fallopian tubes or the ovaries. It has not spread to nearby lymph nodes or distant sites.
Stage IIB: The cancer is on the outer surface of, or has grown into, nearby pelvic organs such as the bladder, the sigmoid colon, or the rectum. It has not spread to nearby lymph nodes or distant sites.
Stage III: The tumor(s) involves one or both ovaries or fallopian tubes, or there is primary peritoneal cancer, with tumor outside of the pelvis and/or within the retroperitoneal lymph nodes.
Stage IIIA1: The cancer is in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer that may have spread or grown into nearby organs in the pelvis. It has spread to the retroperitoneal (pelvic and/or para-aortic) lymph nodes only. It has not spread to distant sites.
Stage IIIA2: The cancer is in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer that has spread or grown into organs outside of the pelvis. During surgery, no cancer is visible in the abdomen (outside of the pelvis) to the naked eye, but tiny deposits of cancer are found in the lining of the abdomen and pelvis when it is examined under the microscope. The cancer may or may not have spread to retroperitoneal lymph nodes.
Stage IIIB: There is cancer in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer that has spread or grown into organs outside the pelvis. The deposits of cancer are large enough for the surgeon to see with the naked eye, but are no bigger than 2 centimeters in size. The cancer may or may not have spread to the retroperitoneal lymph nodes.
Stage IIIC: The cancer is in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer that has spread or grown into organs outside the pelvis. The deposits of cancer are larger than 2 centimeters across and may involve the surface of the liver or spleen. It may or may not have spread to the retroperitoneal lymph nodes, but it has not spread to the inside of the liver or spleen, or to distant sites.
Stage IV: Cancer cells are found beyond the abdomen/pelvis and in other parts of the body.
Stage IVA: Cancer cells are found in the fluid around the lungs (called a malignant pleural effusion) with no other areas of cancer spread such as the liver, spleen, intestine, or lymph nodes outside of the abdomen.
Stage IVB: The cancer has spread to the inside of the spleen or liver, to lymph nodes other than the retroperitoneal lymph nodes, and/or to other organs or tissues outside of the peritoneal cavity such as the lungs and bones.
Treatments for Ovarian Cancer
The treatment for ovarian cancer is customized to each patient and depends on the size and location of the tumor(s), the stage at which the patient is diagnosed, and the patient’s general health. Ovarian cancer care teams may include multiple health care specialists, including primary care providers, medical oncologists, gynecologic oncologists, and radiation oncologists, as well as nurse practitioners, physician assistants, nurses, psychologists, social workers, and rehabilitation specialists. CU Cancer Center doctors offer specialized care for patients with ovarian cancer.
Treatments for ovarian cancer include surgery, radiation therapy, chemotherapy, hormone therapy, and targeted drug therapy. Patients may receive one or more of these treatments in combination. Some patients may also be eligible to participate in clinical trials — doctor-led research studies of new or experimental procedures or treatments.
Surgery for Ovarian Cancer
Surgery is one of the primary treatments for ovarian cancer. There are two goals for surgery in the setting ovarian cancer: staging the disease — determining the extent of tumor (whether and how far it has spread) — and debulking, or removing as much of the tumor as possible. The latter in particular is extremely important for long-term treatment success.
Radiation Therapy for Ovarian Cancer
Radiation therapy uses high-powered energy to kill cancer cells. A doctor who specializes in radiation therapy to treat cancer is called a radiation oncologist. The main type of radiation therapy used to treat ovarian cancer is external-beam radiation therapy (EBRT), which uses a machine located outside the body to focus a beam of X-rays on the area affected by cancer and kill the tumor cells.
Chemotherapy for Ovarian Cancer
Chemotherapy uses drugs to kill rapidly growing cancer cells. Drugs are either injected into a vein (intravenously, or IV) or taken orally (PO). A typical chemotherapy course for ovarian cancer involves three to six cycles of treatment, usually with a combination of two kinds of drugs that are taken together.
Hormonal Therapy for Ovarian Cancer
Used most often to treat ovarian stromal tumors, hormonal therapy uses hormones or hormone-blocking drugs to fight cancer. Hormone therapies for stromal tumors include:
- Luteinizing-hormone-releasing hormone (LHRH) agonists, which turn off estrogen production by the ovaries.
- Tamoxifen, a drug that stops estrogen from stimulating cancer cell growth.
- Aromatase inhibitors, which can help lower estrogen levels in women after menopause and limit the role of estrogen in stimulating tumor growth.
Targeted Drug Therapy for Ovarian Cancer
Targeted therapies focus on the specific genes, proteins, or tissue environments that contribute to ovarian cancer, limiting damage to non-cancerous cells and tissues.
The most common targeted drug therapies for ovarian cancer include:
- Bevacizumab: When cancers grow and spread, they have to create new blood vessels to ensure adequate blood supply. Bevacizumab (Avastin) stops this process by attaching to a protein called VEGF, which typically signals new blood vessels to form. This can slow or stop cancer growth.
- PARP inhibitors: Enzymes known as PARP (poly(ADP)-ribose polymerase) enzymes help to repair damaged DNA within cells. Tumor cells are rapidly dividing and thus at high risk of damaging their DNA. By inhibiting the DNA repair process, these drugs, including agents such as olaparib, rucaparib, and niraparib, make it harder for tumor cells to replicate, which can in turn lead to the death of those cancer cells.
The University of Colorado (CU) Cancer Center partners with UCHealth, Children’s Hospital Colorado, and Rocky Mountain Regional VA to provide clinical care. Please make an appointment with one of our clinical partners to be seen by a CU Cancer Center doctor.
UCHealth Cancer Care - Anschutz Medical Campus
1665 Aurora Court Anschutz Cancer Pavilion
Aurora, CO 80045
720-848-0300
UCHealth Cherry Creek Medical Center
100 Cook Street
Denver, CO 80206
720-848-0000
UCHealth Cancer Center - Highlands Ranch
1500 Park Central Drive
Highlands Ranch, CO 80129
720-516-1100
UCHealth Lone Tree Medical Center
9548 Park Meadows Drive
Lone Tree, CO 80124
720-848-2200
Children's Hospital Colorado:
13123 East 16th Avenue
Aurora, CO 80045
720-777-6740
Rocky Mountain Regional VA Medical Center:
1700 North Wheeling Street
Aurora, CO 80045-7211
303-399-8020
Latest in Ovarian Cancer from the Cancer Center
Loading items....
Information reviewed by Bradley Corr, MD, in October 2025.