Improving Care for Colorado
CU School of Medicine expands access to care statewide
By Mark Couch
(May 2020) The faculty members of the University of Colorado School of Medicine have expanded their outreach to communities throughout the state in the past three years with support from a program that provides federal Medicaid reimbursements for providing care.
Since receiving this support in 2017, University of Colorado School of Medicine providers, who served 122,000 Medicaid patients in the state fiscal year 2016-2017, served over 62,000 additional unique Medicaid members in the first two years of the program, which has enhanced access to primary and specialty services for this historically underserved population. CU faculty now provides care to about one-sixth of the state’s total Medicaid enrollment.
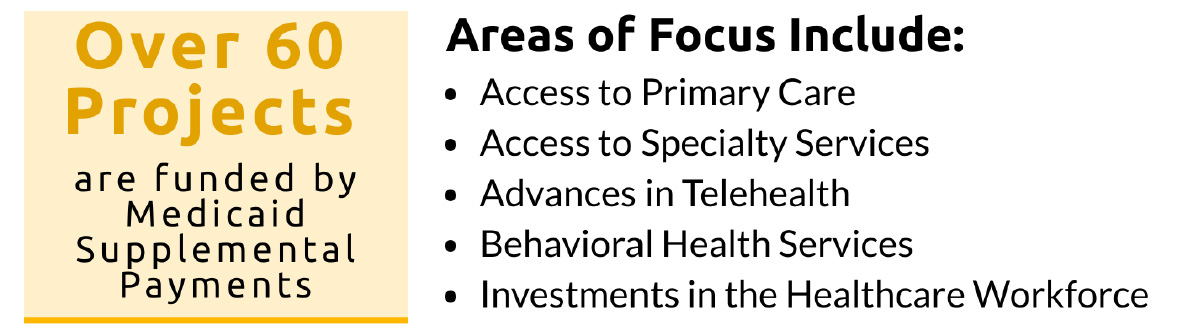
With the expanded support, University of Colorado School of Medicine has established more than 60 projects across the state that are designed to increase access to primary and specialty care, promote evidence-based practices, expand access to underserved rural areas using telehealth, and enhance access to behavioral health services for the Medicaid population.
“Our approach has been to create programming that focuses not just on clinical needs of patients, but also aims to address the social determinants of health and patient barriers to care,” said School of Medicine Dean John J. Reilly, MD. “Our goal has been to make sure Coloradans can remain healthy and that they have access to ways to improve their quality of life. The support we’ve received has been vital to that effort.”
Some projects that receive support are specialty clinics, such as pulmonary and sleep medicine clinics in Grand Junction, Durango, and Cortez, and a student-run clinic in Colorado Springs that provided foot care to the homeless population. In other cases, the support is targeted to programs that build capacity within the health care workforce in local communities, such as ECHO Colorado, which offers innovative distance learning using online, live-video instruction. In 2019, ECHO, which stands for Extension for Community Health Outcomes, connected CU specialists with 570 participants in the state.
The School has also worked closely with state agencies to provide high quality care. The School partners with the Colorado Department of Health Care Policy and Financing to perform analytic projects on patient data to target better interventions and care for patients.
The School also provided continuity of care for those patients who rely on the Health Care Program for Children with Special Needs at six clinics that had been operated through 2018 by the Colorado Department of Public Health and Environment. With Medicaid supplemental funds, the School was able to assume operations at those locations and continue to provide uninterrupted care to patients and families who rely on obtaining those services closer to home.
The overall effort has had a profound impact on care by allowing patients to receive care in their home communities, saving patients a collective 160,000 miles in driving to metro Denver to receive medical care. The funding has created more than 100 jobs for care coordinators, social workers, nurse care managers, and school-based navigators, as well as supporting recruitment of highly specialized physicians in hard-to-recruit subspecialties.
Here are some projects that highlight the scope of what has been created or expanded and that show the range of patients who now have improved access to the high-quality care provided by CU faculty.
Opioid Addiction Care
Even though people with opioid addition were increasingly hospitalized, access to hospital medicine providers with expertise also in addiction treatment was limited.
To address this need for hospital-based physicians with specialized training in addiction treatment, the Department of Medicine Division of Hospital Medicine created a consult service of 11 internal medicine hospitalists who received, through this funding, training in identifying, treating, and supporting patients with substance abuse disorders. From October 2019 to December 2019, the group completed 286 consults.
The 11 hospitalists who were recruited into the addiction medicine training program participated in specialized training and are committed to taking the Addiction Medicine board exam. The training facilitates patients with substance abuse disorders beginning treatment for their addiction while they are in the hospital, rather than waiting for a referral after discharge.
In addition to the specialty training for hospitalists, the program also supports a dedicated social worker and peer recovery coach. Those care providers visited community treatment partners and clinics so that when patients are discharged from the hospital they can be enrolled in programs that provide appropriate care in an outpatient setting.
Children with Autism Spectrum Disorders
Colorado has had a long-established need to provide timely diagnosis and quality care for children with Medicaid who have developmental disabilities and autism spectrum disorders, particularly in rural, frontier, and urban underserved communities.
A program created in 2019 with supplemental Medicaid funding provides rural and frontier provider education opportunities that gives those providers the training needed to do evidence-based diagnoses and offer treatment for developmental disabilities and autism spectrum disorders. One example is training on how to administer the Screening Tool for Autism in Toddlers & Young Children. The training allows earlier intervention, which has been demonstrated to improve long-term outcomes for these children.
These training activities provide a support network that has enabled local primary care providers to identify children with developmental disabilities and autism spectrum disorders early and to then manage behavior. Providers in many Colorado communities, including Edwards, Rifle, Montrose, Grand Junction, Durango, Basalt, Fort Collins, Sterling, and Aspen have received the training.
By providing this training, families can stay in their home communities rather than commute to the Anschutz Medical Campus in Aurora. This model of care reduced a waitlist of 238 school-aged children by 81 percent over an 18-month period and participants from trained practices have a mean wait time reduction from 18 months to two months.
Functional Neurologic Disorders Clinic
The Functional Neurologic Disorders clinic was developed and expanded to provide more accurate diagnosis of non-epileptic seizure patients and provide them with an evidence-based treatment plan and toolkit for continued wellness.
About 25 percent of patients presenting with a seizure diagnosis have a functional neurologic disorder that is better managed through a multispecialty team led by neurologists and psychiatrists providing evidence-based behavioral health interventions. This group of patients has a high rate of using emergency departments for care, but with proper diagnosis and treatment, their reliance on higher-cost emergency room care is reduced.
With supplemental Medicaid funding, the program supports a multidisciplinary team that includes a full-time licensed clinical social worker who delivers direct clinical care. The team also performs community liaison work to care for patients in their primary care medical home and with outside behavioral health care as needed.
The clinic is one of only three such clinics in the western United States. The interventions by the clinic have demonstrated a 75 percent decrease in emergency department use, a 95 percent decrease in in-patient care, and a 91 percent decrease in imaging utilization after treatment.
Statewide Youth Suicide Prevention Initiative
The Colorado Statewide Youth Suicide Prevention Initiative was established to train individuals who work with children and youth
on evidence-based approaches to suicide prevention.
This program engages key stakeholders to design and implement a pilot for establishing a pediatric care pathway that will identify and link youth at risk of suicide to appropriate care.
In 2019, a training associate, content developer, and program evaluator were hired to carry out program development and implementation. This initiative will train those individuals across the state who have contact with nearly all young people in the state. Fully implemented, it is estimated that support will be available to cover 95 percent of the 450,000 children ages 12 years to 17 years in the state of Colorado.
Sickle Cell Treatment and Research Center
The Sickle Cell Treatment and Research Center was established by state legislation in the 1970s with a mission to facilitate health care for those living with sickle cell disease, provide education to providers and the community about sickle cell disease, and to conduct research.
Sickle cell disease is a genetic disorder caused by an inherited abnormality of hemoglobin, the oxygen-carrying protein in red blood cells. The disease is characterized by anemia, acute complications that can become rapidly life threatening, and the development of chronic organ damage.
Limited funding had restricted completion of this mission in some parts of Colorado, so the effort had focused mostly within the service area of the School of Medicine’s partner hospitals on the Anschutz Medical Campus. In recent years, the center faced a growing need from patients in the San Luis Valley in southern Colorado.
With this support, the center was able to develop and sustain a coordinated statewide program offering support to providers in the emergency department, primary care, specialty care, and hospital settings. With improved communication, clinical management guidance, and education across all healthcare systems in Colorado, individuals can seek care where they live from providers who have access to the information necessary to provide care.
Feature Stories
- Building Professional Resilience Through Creative Arts
- Model Hearts and Virtual Reality
- Improving Care for Colorado; CU School of Medicine expands access to care statewide
- New Clinic is ‘Bigger than What’s in These Four Walls’
- Innovative Palliative Care Fellowship Program
- Leadership, Curiosity, Commitment; School of Medicine updates curriculum for medical students
- Student Voice: The Gift of Gratitude
- Faculty Matters: What Every Doctor Should Know About the Holocaust
Profiles
- Searching For Cures to Lung Diseases
- Osseointegration surgery offers hope for better, faster, stronger life
- Building a Team, Not Just a Building; Hospital leader receives life-saving care after stroke at work