Primary Care Diabetes Lab
A multi-disciplinary lab dedicated to ensuring that all people can get the best diabetes preventive practices and treatments, wherever they get their care. We partner with those living with prediabetes, type 1 diabetes, and type 2 diabetes to drive innovations that enhance care.
Diabetes Technologies: We Are All in This Together
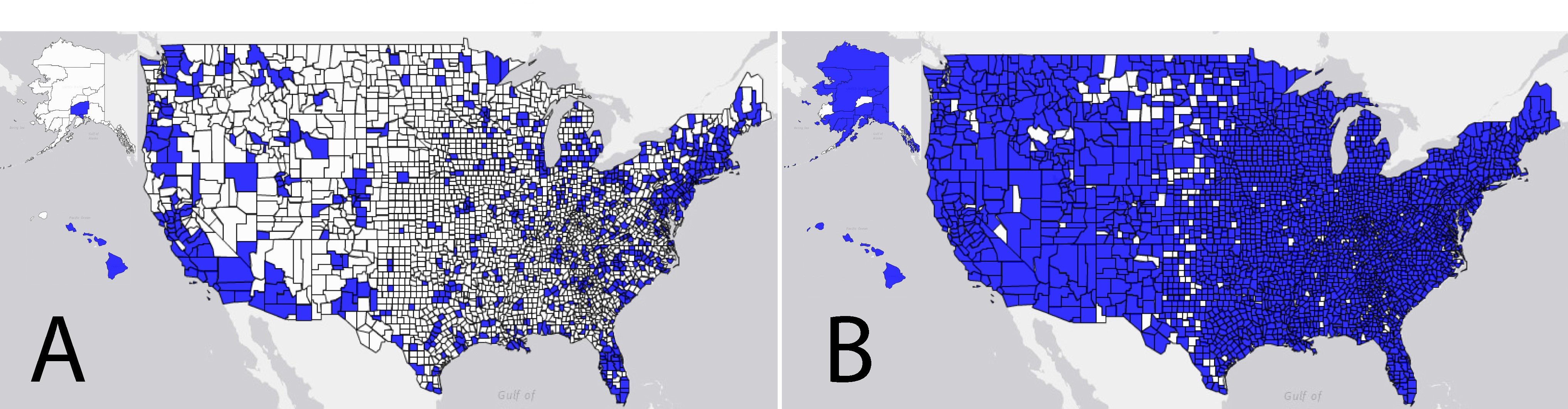
The United States faces a shortage of both primary care physicians (PCPs) and endocrinologists—the two groups of clinicians who provide the majority of care to people with diabetes. Patients treated with intensive insulin therapy, including all of those with type 1 diabetes and many with type 2 diabetes, face numerous daily self-management decisions. These decisions include factoring insulin dosing, glucose management, diet, activity, and other behavioral factors into their decision-making. These patients stand to gain from using the treatment and monitoring technologies that are rapidly advancing and accumulating evidence in support of their benefits. Despite this situation, the actual use of such technologies, including continuous glucose monitoring (CGM) and closed-loop artificial pancreas systems, remains relatively low.
Social Media in the Diabetes Community: a Novel Way to Assess Psychosocial Needs in People with Diabetes and Their Caregivers
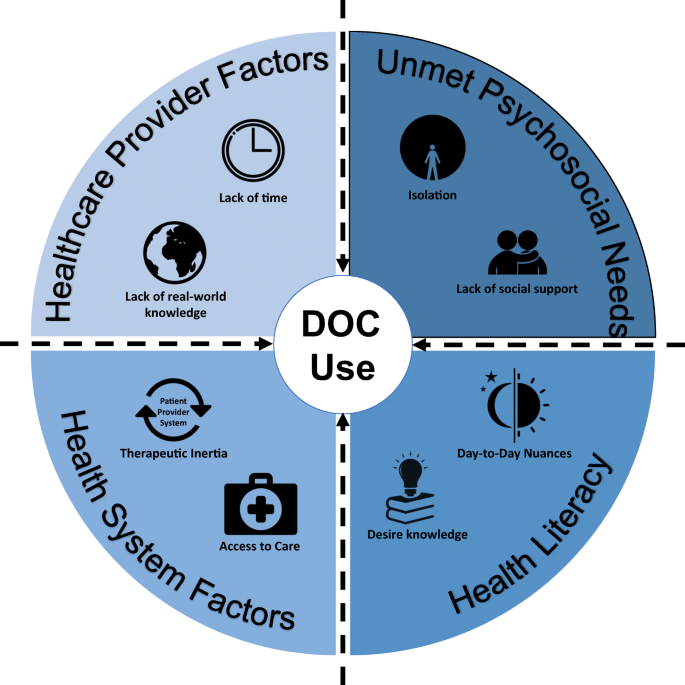
Diabetes is a chronic disease that, regardless of type, requires intensive, ongoing self-management. As a result, people with diabetes (PWD) often have complex environmental, social, behavioral, and informational needs, many of which are unmet in healthcare settings and systems. To help meet these needs, many PWD interact with diabetes online communities (DOCs), including platforms such as Facebook, Twitter, and blogs, to share real-life support, problems, and concerns with other PWD, offering a rich source of data on patient-reported outcomes. This article reviews recent psychosocial needs and outcomes identified by studies of DOCs and/or their users.

Continuous Glucose Monitoring in Primary Care: Understanding and Supporting Clinicians' Use to Enhance Diabetes Care
Diabetes affects approximately 34 million Americans and many do not achieve glycemic targets. Continuous glucose monitoring (CGM) is associated with improved health outcomes for patients with diabetes. Most adults with diabetes receive care for their diabetes in primary care practices, where uptake of CGM is unclear.

Stakeholder engagement in diabetes self-management: patient preference for peer support and other insights
Self-management support (SMS) for patients with diabetes can improve adherence to treatment, mitigate disease-related distress, and improve health outcomes. Translating this evidence into real-world practice is needed, as it is not clear which SMS models are acceptable to patients, and feasible and sustainable for primary care practices.
Determining the Perception and Willingness of Primary Care Providers to Prescribe Advanced Diabetes Technologies
Advanced diabetes technologies have produced increasingly favorable outcomes compared to older treatments. Disparities in practice resources have led to a treatment disparity by clinical setting, where endocrinologists typically prescribe far more such technologies than primary care providers (PCPs). Fully automated artificial pancreas systems (APS), which combine technologies to deliver and adjust insulin dosing continuously in response to automatic and continuous glucose monitoring, may be more straightforward for PCPs to prescribe and manage, therefore extending their benefit to more patients. [...]

Assessing the iLet Bionic Pancreas Deployed in Primary Care and via Telehealth: A Randomized Clinical Trial
The iLet Bionic Pancreas system can improve glycemia in individuals with type 1 diabetes with its simple interface, setup, and maintenance, making it practical for use in the primary care setting and via telehealth. This multisite, random-order crossover trial included 40 adults with type 1 diabetes who received care either from an endocrinology or a primary care clinic and were seen either in person or via telehealth. Average glucose levels were significantly lower among individuals using the Bionic Pancreas compared with usual care in each subgroup.

Challenges and Successes in Raising a Child With Type 1 Diabetes and Autism Spectrum Disorder: Mixed Methods Study
Self-management of type 1 diabetes (T1D) requires numerous decisions and actions by people with T1D and their caregivers and poses many daily challenges. For those with T1D and a developmental disorder such as autism spectrum disorder (ASD), more complex challenges arise, though these remain largely unstudied.

A Novel Approach to Identifying Barriers and Facilitators in Raising a Child With Type 1 Diabetes: Qualitative Analysis of Caregiver Blogs
With rising incidence of type 1 diabetes (T1D) diagnoses among children and the high levels of distress experienced by the caregivers of these children, caregiver support is becoming increasingly important. Historically, relatively few support resources have existed. Increasing use of the Internet, and blogs in particular, has seen a growth of peer support between caregivers of children with T1D. [...]

Peer Support: The Missing Link?
“What doctors overlook is how important it is to simply have emotional support, to know they aren't alone, which inspires people to take care of themselves.” As medical professionals, we may be experts in certain realms of diabetes, but our patients are the experts in living with diabetes. Unless we live with diabetes ourselves, we cannot truly appreciate what it is like to manage the many aspects of diabetes 24/7/365. And every person’s experience is not the same.[...]
Loading items....