Our City
300 days of sunshine
At the foot of the Rocky Mountains, Denver is known for sweeping views and a wide array of outdoor activitiesOur fellowship program provides comprehensive training in the subspecialty of Pediatric Emergency Medicine (PEM). Graduates learn to independently manage all medical conditions that would fall under the purview of a Pediatric Emergency Medicine subspecialist.
Learning from direct patient care is augmented by numerous integrated longitudinal curricula involving research, critical appraisal of literature, quality, toxicology, simulation, EMS/transport, DHEI, self-directed and facilitated educational activities. Our fellows are required to participate in quality projects, lead a scholarship project, produce a first-authored manuscript, and provide education to a variety of trainees, faculty, and medical professionals throughout their fellowship.
Fellows rotate primarily through Children’s Hospital Colorado (Children's Colorado) located on the Anschutz Medical Campus in Aurora, Colorado. Children's Colorado is the only free-standing, quaternary care pediatric hospital in Colorado and the only Level 1 Regional Pediatric Trauma and Burn Center in the state with regional referrals from the surrounding 7-state region.
| Meet the Fellows... | Tour Children's Hospital Colorado... |
Our City
300 days of sunshine
At the foot of the Rocky Mountains, Denver is known for sweeping views and a wide array of outdoor activitiesOur Hospital
Ranked No. 1 in the Rocky Mountain Region
Children’s Hospital Colorado consistently ranks in the top 20 on the U.S. News Best Children’s Hospitals Honor Roll
Our Section
200,000+ Visits Annually
Our large and diverse faculty care for patients presenting with a broad array of conditions
The primary focus of our clinical training is to provide comprehensive training in Pediatric Emergency Medicine (PEM) to allow the graduate to independently manage acutely ill and injured children.

Fellows are directly supervised by Pediatric Emergency Medicine and Emergency Medicine faculty during their clinical ED rotations. Under the supervision of a large and diverse faculty, trainees gain exposure to patients with a broad spectrum of clinical conditions. To prepare trainees to function as effective Pediatric Emergency Medicine subspecialists upon completion of their fellowship, the fellows assume graduated responsibility for patient care over the course of three years.
During their first year, fellows function as direct care providers, focusing on honing clinical and procedural skills. In the second half of the year, fellows will have shifts in which they provide clinical supervision of junior trainees and learn ED management/flow under the direct supervision of a PEM attending.
The First Year for Pediatric-Trained Fellows Includes
For Emergency Medicine-Trained Fellows
During the 2nd half of their second year, fellows begin the transition from caring for patients directly to becoming the supervising physician in charge of an ED team. In their second year, the total amount of clinical time decreases compared to year I and fellows assume more teaching and supervisory responsibilities and dedicate more time to scholarship projects. As part of their clinical requirement, fellows begin “Pre-tending” or “Attending” Shifts where they gradually assume the responsibilities of the Attending ED physician under direct supervision.
The Second Year for Pediatric-Trained Fellows Includes
For emergency medicine-trained fellows, clinical responsibilities during Year 2 transition to 3rd year fellow expectations of Pediatric-trained fellows.
During their third year, fellows become proficient in running a large, urban, Level 1 Trauma Pediatric ED. Fellows take primary responsibility for patients, trainees, and other providers on the ED team, referral and transfer calls, and are expected to maintain an effective working relationship and communication with the charge nurse, nursing and ancillary staff.
The Third Year for Pediatric-Trained Fellows Includes
| 1st Yr Rotation | # Clinical ED Shifts |
|---|---|
| General ED (1 month) | 12 |
| Pediatric Critical Care (1 month) | 0 |
| Peds Anesthesia (1 month) | 4 |
| Toxicology (1 month) | 6 |
| Research (1 month) | 8 |
| PEM ED shifts (6 months) (Includes 2-week Ultrasound Block) | 90-100 |
| Totals | 108-118 PEM ED Shifts 12 Adult ED Shifts |
| 2nd Yr Rotation | # Clinical ED Shifts |
| General ED | 12 |
| EMS/Transport | 2-6 |
| Research (6 months) | 40-48 |
| PEM ED (2 months) | 28-32 |
| Electives | 3-6 |
| Attending shifts (2nd semester) | 14 |
| Totals | 100-110 PEM ED Shifts 12 Adult ED Shifts |
| 3rd Yr Rotation | # Clinical ED Shifts |
| General ED | 12 |
| Elective (1 month) | 0 |
| Adult ED POCUS (1 month) | 6 |
| Research (5 months) | 40 |
| PEM ED (4 months) | 48-58 |
| Totals | 88-98 PEM ED Shifts 18 Adult ED shifts |
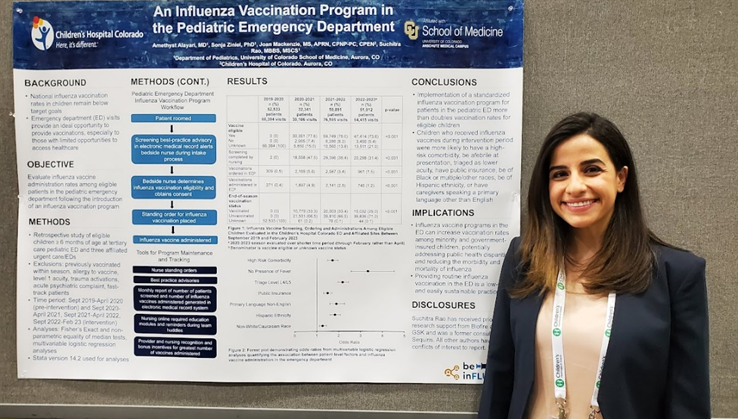
The program provides comprehensive scholarly training that prepares all trainees with the background and skills to compete for academic faculty positions at the completion of their fellowship.
Graduates are expected to complete a scholarly project during their three years including presentation of the project at a national meeting, such as the American Academy of Pediatrics fall meeting or the Pediatric Academic Societies spring meeting, and submission of a first-authored manuscript to a peer-reviewed publication. Fellows are also required to be involved in QI.
The Section has a full-time research coordinator and biostatistician who are available for assistance with study design, IRB applications, database management, statistical analysis, and grant submissions.
Fellows have access to Professional Research Assistants (PRAs) who can assist with study enrollment and data collection in the Children’s ED. PRA coverage averages 10-16 hours per day.
*Emergency Medicine-trained PEM fellows have a 2-year curriculum. The scholarship project requirements are the same regardless of training path.
Pediatric Emergency Medicine fellows are encouraged to attend national scientific meetings throughout their fellowship. If funding is available, the Section supports travel to any national meeting for which the trainee has an abstract or platform presentation according to section guidelines.
The University of Colorado Denver/Children's Colorado is a member of PECARN, the Pediatric Emergency Care Applied Research Network. PECARN is a federally funded pediatric emergency medicine research network conducting multi-institutional research on the prevention and management of acute illness and injuries in children and youth of all ages. For more information, visit http://www.pecarn.org/
Several faculty are members of PEM CRC, the PEM Collaborative Research Committee, a subcommittee of the American Academy of Pediatrics Section on Emergency Medicine. PEM CRC is an unfunded volunteer effort which provides a framework for multicenter investigation. It provides a means of developing protocols and identifying interested co-investigators at over 40 member sites. For more information, visit http://www.pemcrc.org/
The Colorado Clinical and Translational Sciences Institute (CCTSI) is a collaborative enterprise between University of Colorado Denver, University of Colorado at Boulder, six affiliated hospitals and health care organizations, and multiple community organizations with resources to promote research and training that will advance health care and improve the public health. Through the CCTSI, Clinical Translational Research Centers (CTRCs) have been established at several affiliated hospitals, including Children's Colorado, University of Colorado Hospital, and Denver Health Medical Center. The CTRC also offers biostatistical collaboration/consultation for study design, including sample size and power calculations, and data analysis. Colorado Child Health Research Institute CCHRI) also offered limited research support to fellows.
Learning from direct patient care is augmented by a comprehensive series of lectures and conferences focused on Pediatric Emergency Medicine and associated longitudinal curricula.

Fellows participate in several educational seminars focused on Pediatric Emergency Medicine. Most education takes place during mandatory sessions on Thursday that anchor the educational program.
| Ultrasound Curriculum | |
 |
|
| Simulation Curriculum | |
 |
|
New to our curriculum are optional fellowship tracks designed for those fellows who desire additional training with concentration in the following areas:
These tracks have specific mentored scholarship requirements, supplemental coursework, and educational/teaching responsibilities in addition to regular series fellowship curriculum requirements.

Quarterly dinners hosted by faculty to discuss specific topics such as career, wellness, and resiliency.
Fellows have the opportunity to apply for an 8-hour session by The Institute for Healthcare Quality, Safety and Efficiency (IHQSE) that covers the importance of quality science in health care, basic tools for analyzing processes of care and identifying opportunities for improvement, fundamental data collection and analysis techniques to support quality improvement projects, methods for creating and testing potential changes, and tactics for implementing and spreading improvement ideas.
Subspecialty Excellence in Educational Leadership & Scholarship (SEELS) Program
The University of Colorado Department of Pediatrics is proud to offer the Subspecialty Excellence in Educational Leadership & Scholarship (SEELS) Program for subspecialty pediatric fellows committed to an academic career in medical education.
The SEELS program guides fellows through an 18-month program that provides research mentorship, coaching, and instruction.
The overall goal of SEELS is to equip these fellows with the necessary knowledge/skills/attitudes for success as future medical educators through educational scholarship and professional identity development, faculty and peer mentorship, and engaging in an educational community of practice.
Pediatric Fellowship Educational Series
This educational series has been developed by the Committee on Fellowship Education to address areas of scholarly interest common to all pediatric fellows. Nearly 100 sub-specialized physicians in training will attend 5-6 half-day seminars spread across their 3 years of fellowship.
Pediatric Biostatistics for Clinicians Course
This course is primarily intended for 2nd and 3rd year Department of Pediatrics fellows as part of the comprehensive fellowship educational program. Designed to help fellows to develop an ability to be a critical consumer of the literature and develop familiarity with many commonly used statistical methods.
Masters of Science in Clinical Sciences (MSCS) program is offered through the university and select fellows through the Department of Pediatrics may apply for limited funding support for this program if grants are available.
A mini-certificate or a Masters of Public Health (MPH) degree may be obtained at the Colorado School of Public Health (collaboration between University of Colorado Denver, Colorado State University and the University of Northern Colorado). The certificate program requires 15 hours of graduate work and the MPH requires 42 hours of graduate work. This requires extra time commitment as the clinical and elective requirements remain unchanged. Funding for trainee graduate coursework is not supported by the section of emergency medicine.
*indicates required teaching opportunity

1st Year Fellows | |
Abby Kathryn Fahnestock, MD |
|
Sara Nicole Kirkpatrick, DO |
|
Rohan Rao, MD |
|
Laura Elizabeth Wylie, MD |
|
2nd Year Fellows | |
Chelsea Lauren Clarke, DO |
|
Crystal Amber Dickson, MD |
|
Keren Eyal, MD, MPH |
|
Jeremiah Thurgood Lowe, MD, MS |
|
3rd Year Fellows | |
Alexandra Berardi-Bloomfield, MD |
|
Savannah Adelaide Zoe Brackman, MD |
|
Erica K. Sheline, MD
|
|
Margaret Elizabeth Tashjian, MD
|
|
| Academic Training Facility/Institution | Faculty (Private Community) | Continuing Education/ Fellowship | Military/Other |
|---|---|---|---|
| 83% | 7% | 7% | 4% |

All application material should be submitted through the Electronic Residency Application Service(ERAS) by July 31st. Applications received after this date will not be considered due to the large number of applicants and short interview season. We participate in the National Residency Matching Program (NRMP) and typically do not offer any positions outside of the match. Required application materials include:
| Date | Activity |
| Monday, May 31, 2026 | ERAS 2026 season ends at 5 p.m. ET. |
| Wednesday, June 3, 2026 | ERAS 2027 season begins at 9 a.m. ET. |
| Thursday, June 4, 2026 | EFDO will release tokens to fellowship applicants. |
| Wednesday, July 1, 2026 | July cycle fellowship applicants may begin submitting applications to programs at 9 a.m. ET. |
| Wednesday July 15, 2026 | July cycle fellowship programs may begin reviewing applications at 9 a.m. ET. |
| May 31, 2027 | ERAS 2027 season ends at 5 p.m. ET. |
| Dates | Activity |
| Wednesday, August 26, 2026 | Match Opens |
| Wednesday, September 30, 2026 | Ranking Opens |
| Wednesday, October 28, 2026 | Quota Change Deadline |
| Wednesday, November 18, 2026 | Rank Order List Certification Deadline |
| Wednesday, December 2, 2026 | MATCH DAY |
Applications will be accepted as soon as the ERAS opens to programs in mid-July. Applications must be submitted before July 31st. Due to the large number of applicants, we will not be reviewing applications submitted after this time or applications which are significantly incomplete may not be considered. Additional dates for the Pediatric Emergency Medicine fellowship match are provided below.
Our program will be conducting all-virtual interviews this season. Communications from the program will either come through ERAS or to the applicant’s designated email address. Applicants will be notified of their status by August 15th. The Department of Pediatrics may offer in-person visits for fellowship interviewees after the program rank list has been submitted. Applicants will be notified of these opportunities if they arise and can visit the city or campus on their own. Program representatives will not meet with applicants outside of these official opportunities.
Fall Interview dates are typically on Wednesdays in September and October.
If you have questions regarding the application process, please contact our program coordinator, Jessica Coleman via email at [email protected].
Do not send messages to the program through ERAS.
The University of Colorado offers salary and benefits packages that are competitive with other fellowship programs across the country. Current salary levels can be found at the School of Medicine - Graduate Medical Education Stipends
| Please address further questions to: | |
 | Tien Vu, MD
|
 | Jason Woods, MD
|
 | Jessica Coleman
|
Pediatric Emergency Medicine Fellowship
Program Coordinator: Jessica.Coleman
13123 East 16th Avenue, Box
Aurora, CO 80045
Phone: 303-724-2566 | Fax:720-777-7258