CUSOM Trek: Our process of reform
Learning Theory in the Trek Curriculum
By Paige Romer, MA, MS2
(September 2021) During the first week of orientation, Trek students completed a session called Learning How to Learn Medicine, in which they discussed several key topics from learning theory and how those topics would be relevant to them in medical school.
The session covered the following concepts and presented concrete strategies for how to implement these best study practices within the Trek curriculum.Different Types of Memory
Working memory is the memory system that is used when you are actively thinking about a topic or learning it for the first time. Recent research has shown that the average person can hold approximately four pieces of information or four chunks (more on this later) in their working memory. Long-term memory is where information is stored for later use. The process of moving information from short-term memory to long-term memory is called encoding. The process of moving information from long-term memory to short-term memory is called retrieval. For students, one of the most effective ways to strengthen long-term memory is retrieval practice, or the process of recalling information out of long-term memory and into short-term memory by self-testing.
Chunking
Chunks are pieces of information that are bound by meaning or use. Examples of chunks that students will create in medical school are the glycolysis pathway, a pediatric cough differential diagnosis, blood flow patterns in the upper-limb, and the process of suturing. Chunking is important because it allows us to increase our working memory capacity. By holding four chunks instead of four discrete pieces of information in the working memory, we can make new connections and develop deeper understanding.
Learning Illusions
Learning illusions are activities that feel like learning, but do not involve true encoding or retrieval. Examples of encoding are rereading notes multiple times, highlighting a textbook, or rewatching a video on the same topic multiple times. When we engage in these activities, our working memory tricks us because it recognizes familiar information, but no encoding actually happens. In the Learning How to Learn Medicine session, students discussed strategies that could be used in place of learning illusions, including rewriting notes from memory rather than rereading them or making flashcards while watching a video to later be used for retrieval practice.
Interleaving
Interleaving is the process of switching between different topics as you study. Interleaving creates stronger neural connections and allows for less obvious, more creative connections to be made between topics. It ultimately leads to better and more durable understanding along with flexible thinking skills.
Spaced Repetition
Spaced repetition is the process of self-testing on material over increasing intervals of time, rather than cramming and learning all the information at once. Spaced repetition has been shown to be one of the most effective ways of beating the forgetting curve, which shows that roughly 50% of new information is forgotten within a day of learning it if no retrieval practice occurs.
In the Learning How to Learn Medicine session, students were asked to consider times in their lives that they had used each of the above learning theories in the process of acquiring a skill. They each walked away with a plan for how to incorporate these strategies into their study practices.
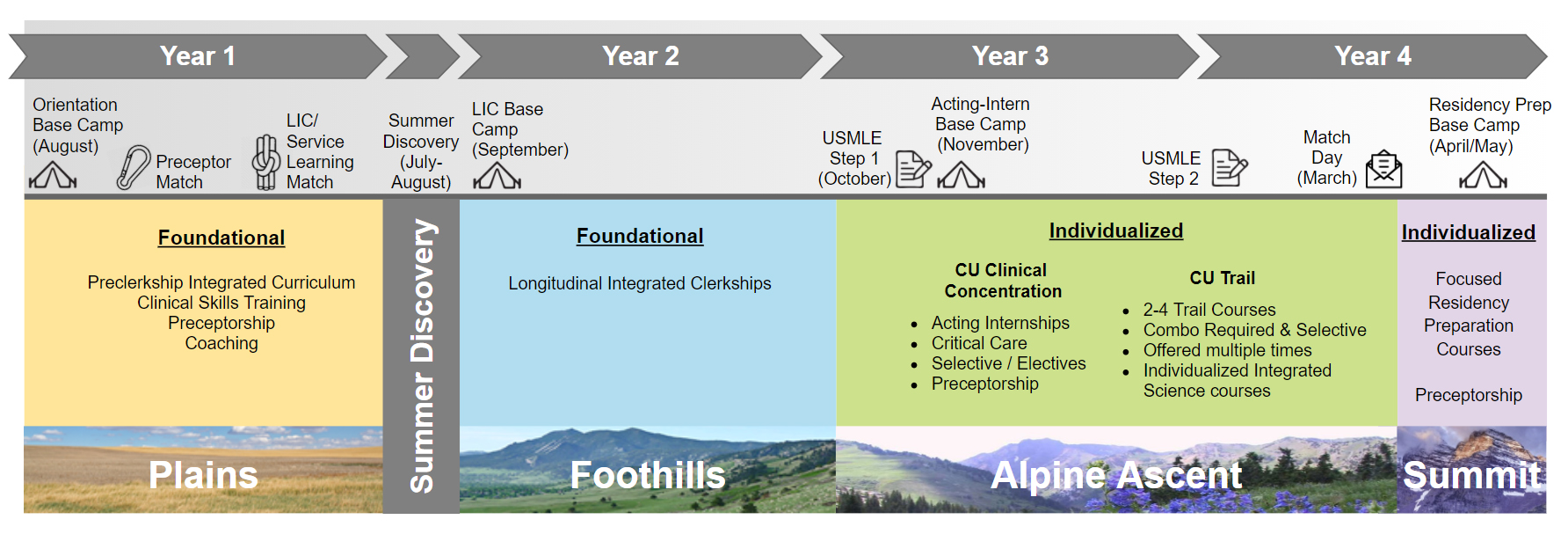
During the session, students were also able to see how these theories are already woven into the Trek curriculum. For example, the LIC (Longitudinal Integrated Clerkship) model involves both interleaving and spaced repetition by having students switch between different disciplines throughout the week and spreading their learning out over the space of the entire clinical year. Additionally, the Plains curriculum involves interleaving by integrating the clinical sciences and medical sciences throughout each block.
The incorporation of learning theory into the Trek curriculum design will provide students with the opportunity to build the skills that will allow them to be successful, curious and joyful lifelong learners.
Office of Student Life Contact Information
| Mailing address: 13001 East 17th Place, Mail Stop C292, Aurora, CO 80045 School of Medicine Undergraduate Medical Education Document Requests Page |
Vision: Our graduates will be physician leaders capable of transforming the health of diverse communities.
Mission: Through a longitudinally integrated curriculum, we aim to educate physician leaders who are curious, life-long learners with a commitment to serve the profession, our patients, and society.
Values/Pillars: Leadership, Curiosity, Commitment
Mission: Through a longitudinally integrated curriculum, we aim to educate physician leaders who are curious, life-long learners with a commitment to serve the profession, our patients, and society.
Values/Pillars: Leadership, Curiosity, Commitment
Did You Know?
- The University of Colorado School of Medicine was founded in 1883
- The last major curriculum reform was implemented in 2006
- Over 150 people attended the most recent curriculum reform kickoff in October 2017
- Over 200 people: faculty, students, and community members are currently serving on Curriculum Reform subcommittees