Our City
Denver is known for its beautiful weather, sweeping views, excellent city life, and an array of outdoor activities courtesy of our proximity to the magnificent Rocky MountainsMedical Genetics & Genomics Residency Program
Overview
We offer the ACGME-accredited categorical Medical Genetics and Genomics (MGG) Residency Program and the combined Pediatric/Medical Genetics and Genomics (Peds/MGG) Residency program at the University of Colorado. These programs offer trainees the opportunity to expand their knowledge as physicians in the field of pediatric medical genetics. Providing clinical services at The Children’s Hospital Colorado, the section follows a large number of patients from Colorado, Wyoming, Montana, and parts of Nebraska, Kansas, and New Mexico. This large patient catchment area has allowed us to care for kids and adults with a broad variety of genetic disorders. Staffed by clinicians and a team of outstanding genetic counselors, nurses, and dieticians, our trainees have the opportunity to work with a diverse array of specialist in the field.
Trainees have access to the broad course offerings of the School of Medicine and a curriculum in the scientific underpinnings of clinical genetics is offered through the M.S. in Human Genetics and Genetic Counseling program. The MGG program is 2 years in length; the Peds/MGG program is 4 years in length, both have a complement of 2 per year and prepare graduates to sit for the Clinical Genetics Board Examination administered by the American Board of Medical Genetics (ABMG).
The programs seek to attract physicians from diverse backgrounds and experience interested in pursuing careers in medical genetics. Eligible MGG candidates must have an MD or DO and have completed at least 1 year of residency training in another ACGME-accredited primary specialty in the United States or equivalent training in Canada; Peds/MGG candidates must have completed an MD or DO from a US or Canadian school or have current ECFMG certification. Trainees must be eligible to work in the United States and obtain a Colorado medical license before the commencement of training.
Clinical medical geneticists are able to:
- Diagnose and manage genetic disorders
- Provide patient and family counseling
- Use their knowledge of heterogeneity, variability, and natural history of genetic disorders in patient care decision-making
- Elicit and interpret individual and family medical histories
- Interpret clinical genetic and specialized laboratory testing information
- Explain the causes and natural history of genetic disorders and genetic risk assessment
- Interact with other healthcare professionals in the provision of services for patients with genetically influenced disorders
Our Hospital
Children's Hospital Colorado consistently ranks in the top 20 on the US News Best Children's Hospitals Honor Roll and as the #1 Children's Hospital in Colorado and the Rocky Mountain regionOur Department
We evaluate, diagnose and help treat children and families affected by sporadic and inherited genetic disorders, birth defects, or developmental delaysOverview
The overall goal of the program is to train highly competent, clinical medical geneticists who are able to provide state of the art level of diagnostic, management, and counseling services for wide variety of genetic disorders. The resident’s assignments during the 2 year genetic residency are based on each activity’s educational value toward achieving the program objectives and are not dictated by the service needs.
This 2 year program is divided into twelve 1 month block rotations per year.
Residents will spend 12 months in the genetics and metabolics clinics at Children’s Hospital Colorado. During these months, residents will have primary responsibility for preparing for clinic visits, conducting visits and then ensuring that appropriate follow up is provided. In addition to general metabolic and general genetics clinics, residents will attend the following specialty clinics: lysosomal, mitochondrial, PKU, galactosemia, skeletal dysplasia, neurogenetics, autism, Prader Willi, Angelman, 22q, neurofibromatosis, ocular genetics, vascular malformations.
Residents will spend 6 months in the University Hospital genetics clinics. This includes the Adult Genetics clinic, prenatal genetics as well as adult hereditary cancer syndromes clinic. During those months, residents will also participate in prenatal genetics consultations at Children’s Hospital Colorado as well as participating in the pediatric hereditary cancer syndromes clinic.
Residents will spend 3 months conducting a research project of their choosing under the mentorship of one of the faculty members. Those months may be arranged as is most conducive to the particular project (either consecutively or dispersed).
Residents will spend 6 weeks of time in the 3 affiliated laboratories (biochemical, molecular genetics, cytogenetics). They will also spend 6 weeks attending elective clinics such as cardiac genetics, neuromuscular clinic, Down syndrome clinic, fragile X clinic, hearing loss clinic, and craniofacial clinic.
Residents will spend 1 week of each month on call for the inpatient genetics and metabolics service at Children’s Hospital Colorado.
Responsibilities during the monthly week on call include:
- first call for inpatient consultations
- first call for outpatient consultations from internal and community physicians
- conduct urgent add-on clinic visits
- participate in newborn screen results follow up
- take urgent calls from families about management of illness
Overview
The residents have a 6 week laboratory rotation which includes 2 weeks each in the cytogenetics laboratory, molecular genetics laboratory, and biochemical genetics laboratory.
The goal of these rotations is for the residents to:
- learn what techniques are used for the diagnostic tests and what specimen is appropriate for each test.
- learn the interpretation of the results in regard to its clinical. significance and to learn what other tests are indicated to clarify any ambiguity or further define an abnormality.
- become aware of the regulations and guidelines under which a laboratory is required to operate.
- become proficient at reporting laboratory results back to the ordering care providers.
- become familiar with laboratory workflow and administration.
Cytogenetics Lab
This lab is a full-service state of the art clinical cytogenetics, molecular genetics, education and research laboratory. With a rich history as a leader, early milestones included automated karyotyping (1986), clinical fluorescent in situ hybridization (FISH, 1991), and comparative genomic hybridization (CGH, 1992) in addition to standard cytogenetic testing. Clinical sample volume approaches 12,000 samples/year of postnatal, prenatal, and cancer including paraffin embedded samples. Rapidly expanding chromosomal microarray (CMA) genomic testing has been offered clinically since 2006, with a high density CMA/SNP array since 2014.
Molecular Lab
This lab has become a worldwide referral center for molecular testing for inborn errors of metabolism, pigmentation disorders, and diseases of the eye in addition to offering testing for common disorders such as the Fragile X syndrome, cystic fibrosis and thrombophilia. The lab currently process approximately 3500 samples per year and offers testing for over 150 genes. It serves as a core center for isolation of DNA from blood and other tissues for many projects on the Anschutz Medical Campus, including the CTSI. Advanced molecular testing, such as duplication/deletion chips and exome sequencing, are in development.
Biochemical Genetics Lab:
This lab focuses on procedures relevant to the diagnosis and management of amino and organic acidemias and disorders of fatty acid oxidation. Analyses presently offered include amino acid screening and quantitation; organic acid screening; quantitation of succinylacetone and glutaric, 3-hydroxyglutaric, orotic, methylmalonic, and N-acetyl aspartic acids by stable isotope dilution gc-ms; screening and qualitative analysis of mucopolysaccharides; profiling of acylcarnitines by tandem mass spectrometry; and enzyme assays for very long-chain acyl-CoA dehydrogenase, glutaryl-CoA dehydrogenase, electron transfer flavoprotein (ETF), and ETF-ubiquinone oxidoreductase. The laboratory has been CAP accredited for over twenty years.
Didactic Lectures Overview
Didactic Lectures
We offer several didactic courses to trainees, including:
- MBG Core Clinical Seminar Series (launched in 2020, this online conference spans several months & includes experts in the field across the US)
- Molecular Genetics and Cytogenetics
- Survey in Human Genetics (offered through the Human Medical Genetics Program)
- Biochemical Genetics
- Risk Assessment
- Cancer Genetics
The classes are coordinated through the graduate genetic counseling program except where noted above. Further, the Department of Pediatrics offers an evening fellows lecture series to which the medical genetics residents are invited and encouraged to attend.
Conferences
Residents participate in the following education conferences:
- Basic science research presentations
- Metabolic patient care meeting
- Laboratory Rounds
- Pediatric Grand Rounds
- Genetics Journal Club
- Genetics Grand Rounds
- Variant interpretation conference
- Clinical research update meetings
- Morbidity and Mortality Conference
- Radiology Rounds
Scholarly Activities
In addition to the formal research rotation, the residents are encouraged to participate in scholarly activities throughout the 2 years of residency. Attendance and submission of abstracts or presentations to local, regional, or national meetings is encouraged.
Other Opportunities:
- QI/QC Workshop and training
- Resilience training
- Resident and fellow retreats/workshops through GME
- Metabolic University
- Mountain States Regional Genetics Network Meeting
- North American Metabolic Academy (NAMA)
Difference
The University of Colorado’s School of Medicine, the Children’s Hospital Colorado, and the Heart Institute believe that diversity is a value that is central to their educational, research, service and health care missions. We are committed to working towards equity and justice for all.
Diversity in Denver
Training at the University of Colorado provides the opportunity to care for an incredibly diverse population of patients and families. As the regional referral center for the Mountain West, Children’s Hospital Colorado and the Heart Institute regularly serves children from urban and rural areas in multiple states including Colorado, Wyoming, Montana, New Mexico, Nebraska, Kansas, and North and South Dakota.
The Denver Metro Area is home to a diverse and vibrant array of people from all racial, ethnic, socioeconomic, religious, and cultural backgrounds. Denver is one of the fastest-growing cities in the United States with a city population of over 700,000 and over 3 million in the metropolitan area. Approximately 1 in 6 Denver residents was born in a country other than the United States and over 40% of children in Denver speak a language other than English at home. The population of Denver is approximately 1% Native American, 5% Asian, 12% Black, 50% non-Hispanic White, and 32% Hispanic/Latinx. In the three-zip-code region surrounding the Children’s Hospital Colorado, 77% of residents belong to racial and ethnic minorities. In addition, Denver ranks among the top 10 cities in the United States for the highest proportion of residents who identify as LGBT.
University of Colorado and Children’s Hospital Colorado DEI Resources:
- University of Colorado Anschutz Medical Campus Central Office of Diversity, Equity, Inclusion, and Community Engagement
- Pediatric Residency Program – Diversity and Inclusion
- Diversity in Pediatrics Committee
- Minority and Allied Resident Council (MARC)
The CU Anschutz LGBTQ+ Hub
Repurposes the Women and Gender Center formerly at CU Anschutz. On this website you will find information about services and resources provided by the LGBTQ+ Hub.
You can also visit us in our physical space (shared with the Oasis Space) Mondays, Wednesdays, and Fridays, located on the second floor of the Education 2 North Building, room 2101.
Here is the website link: https://www.cuanschutz.edu/offices/diversity-equity-inclusion-community/programs-and-initiatives/lgbtq-hub
Current Residents

Hometown: Hamden, CT
Medical School: Vanderbilt
Research Interest(s): electronic health record/biobank research
Other Interest(s): hanging out with my partner and our cats, playing board games, knitting/crochet

Hometown: Prineville, OR
Medical School: Baylor College of Medicine
Research Interest(s): Pharmacogenomics, Medical Education
Other Interest(s): Pickleball, Cycling, Trail running, Nuclear Physics

Hometown: Portland, Oregon
Medical School: Washington State University
Research Interest(s): Gene therapy, Metabolic disorders, AI in medicine, flok.org
Other Interest(s): Running/triathlons, Exploring the mountains, Dogs (especially Labs), Salty ice cream (is this a Colorado thing?), Flok Family Camp (fun times with my community!), Rockies games, visiting nice zoos (Denver zoo and Cheyenne Mtn Zoo are phenomenal!)

Hometown: Flower Mound, Tx
Medical School: University of Texas Medical Branch
Research interests: clinical trials, developmental pediatrics
Other interests: skiing and cycling!

Maria Aleja Gonzalez Rodriguez, MD
Hometown: Bogotá, Colombia
Medical School: Universidad del Rosario
Research Interest(s): Hereditary tumor syndromes, Inherited Metabolic Diseases
Other Interest(s): Running, Photography, Dancing

Hometown: Tuttle, Oklahoma
Medical School: University of Oklahoma College
Research Interest: Mitochondrial function & Aging. Genetics of autoimmune disease.
Interest/Hobbies: Camping, Hiking, Karaoke, Gym, Getting a sweet lil' treat, Playing Magic: the Gathering with the boys, Hot girl walks, Arcade bars, Watching OKC Thunder, Leaving Restaurant Yelp Reviews
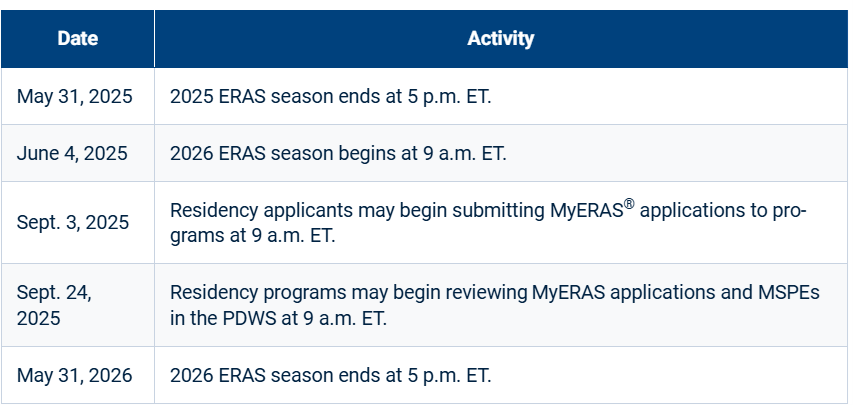
All applications are received through ERAS.
The Application Process
Our pediatric fellowships will be conducting virtual interviews for this upcoming interview season. We will be interviewing to fill two combined residency spots for the 2024 academic year. We look forward to sharing our programs with you and getting to know more about you. We will send interview offers out early-October as well as a list of interview dates in October, November, and early December.
If you have questions about the application process, please feel free to reach out to our program coordinator! (Sara Higsley: [email protected])
We particularly hope to attract applicants who are motivated and self-directed learners who want to develop academic careers based on excellence in research, scholarship, and clinical pediatric genetics. The Medical Genetics and Genomics Program utilizes ERAS - Electronic Residency Application Service (ERAS).
We participate in the National Residency Matching Program (NRMP) and do not offer any positions outside of the match. The application should include a copy of your curriculum vitae, at least 3 letters of reference (maximal of 4), a personal statement highlighting why you wish to become a pediatric cardiologist, and your USMLE or COMLEX score reports. If you are not a US citizen, include a copy of your ECFMG report with ERAS. Please bear in mind that you would need to acquire a J1 visa if selected as a candidate for our program. Incomplete or late applications will not be considered. It is your responsibility to ensure all required information has been received.
ERAS Application Timeline
NRMP Main Residency Match Timeline
| Date | Activity |
|---|---|
| September 15, 2025 | Registration Opens |
| January 30, 2026 | Standard Registration Deadline |
| February 2, 2026 | Ranking Opens |
| March 4, 2026 | Rank Order List Certification Deadline |
| March 20, 2026 | Match Day! |
Salary and Benefits
The University of Colorado offers salary and benefits packages that are competitive with other fellowship programs across the country. Current salary levels can be found at the School of Medicine - Graduate Medical Education Stipends.
Denver
The Mile High City is nestled at the eastern base of the Rocky Mountains and is the largest city in the region with a population of over 2.7 million. Denver enjoys one of the best climates in the country, with 300 days/year of sunny skies. Although it snows in the winter, the snow melts quickly and temperatures are usually moderate. Hot summer days give way to cool summer evenings. The city is the home to dozens of highly rated restaurants and a vibrant nightlife. The city attracts many outdoor enthusiasts with its extensive system of hiking and bike trails and the largest city park system in the country. The Denver Center for the Performing Arts is the largest performing arts complex under one roof in the country and attracts many of the top national theater tours each year. Red Rocks Amphitheater, a natural amphitheater in the foothills west of town, attracts the nation’s top touring musical talent throughout the summer.
Denver is home to the Denver Broncos (NFL), the Denver Nuggets (NBA), the Colorado Rockies (MLB), the Colorado Avalanche (NHL), the Colorado Rapids (MLS) and the Colorado Outlaws (MLL). The University of Colorado, the state flagship school and a world-class educational institution, is based in nearby Boulder. In addition, Denver is the gateway to the Rocky Mountains, which offer abundant recreational and sightseeing opportunities year round. The state of Colorado is home to over 20 major ski areas, many of which are within 2 hours of the city.
Virtual Interviews
In accordance with the University of Colorado Anschutz Medical Campus, we will be conducting our 2024 interviews virtually over zoom. We are so excited to meet you (virtually!) and help you get to know our program. Below you will find the schedule for your interview day. We will be holding our interviews on Mondays and Tuesdays in October, November, and December.
| 1:00pm-1:45pm (MST) | Interview with Current Resident |
| 2:00pm-2:45pm (MST) | Interview with Genetic Counselor or Research Faculty |
| 3:00pm-3:45pm (MST) | Interview with Faculty Member |
| 4:00pm-4:45pm (MST) | Interview with Program Director or Associate Program Director |
Additional Questions
Please contact with questions:
Sara Higsley, Fellowship Program Coordinator: [email protected]
Aaina Kochhar, MD, Program Director: [email protected]
Farrah Rajabi, MD, Associate Program Director: [email protected]