Center for Rare Melanomas Newsroom
-

Our mucosal melanoma patient survey is LIVE!Opens in a new window
Mar 1, 2024One of the most commonly asked questions by mucosal melanoma patients is "why did I develop this disease???" Cancers can be caused by genetic risk factors (think a germline mutation passed down and multiple family members affected), environmental factors (think radon exposure, chemical exposures at work), and/or lifestyle factors (think smoking, HPV in cervical cancer). While clinicians and researchers have access to genomic DNA from patients to evaluate genetic risks, the only way we can study environmental and lifestyle factors is by getting that information directly from PATIENTS! Given the particularly sensitive nature of lifestyle factors that may impact vulvovaginal and/or anorectal melanomas, we felt an anonymous survey is the best way to obtain this information. Our survey is a two-part survey: first, patients anonymously complete their survey on environment and lifestyle hisotry. Then, they get a unique ID number to give to their oncologist to complete a second survey anonymously (the oncologist does not see any patient survey answers), which provides clinical information that is sometimes hard for patients to answer. We have an initial goal of 250 participants, and hope this data will provide some knowledge that can contribute to prevention and earlier detection of mucosal melanoma. If you are a patient, please take our survey and help spread the word! And, if you are a treating oncologist, please take the extra time to complete the important follow up survey.Opens in a new window Full story -
Proceedings from the MRF sponsored Mucosal Melanoma Workshop are published!Opens in a new window
Nov 1, 2023Collaboration is key when it comes to clinical and translational research for rare diseases. Out of all the "rare" forms of melanoma, mucosal melanoma is truly the rarest of the rare as it only accounts for ~1% of malignant melanoma cases. To date, mucosal melanoma research is lagging behind all other melanoma subtypes. In order to boost collaboration within the mucosal melanoma community, the Melanoma Research Foundation (MRF) sponsored a one-day workshop at Columbia University on December 15, 2022. The workshop, "Increasing collaboration amongst the mucosal melanoma community" brought together clinicians, researchers, and patients in a first-of-its kind meeting focused solely on mucosal melanoma and how we can work collaboratively moving forward to launch mucosal melanoma based research findings from risk factors to effective therapies. The published article provides a review of mucosal melanoma, an overview of the topics and talks given during the workshop, and a compass of which direction the field needs to head as we move forward toward better understanding and treatments for mucosal melanoma.Opens in a new window Full story -

Clinical Trial for Patients with Mucosal Melanoma- Now Enrolling at University of ColoradoOpens in a new window
Dec 1, 2022Earlier this year, the CU Center for Rare Melanomas launched a clinical trial for patients with advanced mucosal melanoma. This trial combines the epigenetic modifying drug Decitabine, "DEC-C", with Nivolumab anti-PD-1 immunotherapy. Activation of the RIG-I innate immune pathway and increased expression of tumor antigens and pro-immune genes by DEC-C during Nivolumab treatment may enhance the frequency and activity of anti-tumor immune cells (CD4+ and CD8+ T-cells, NK cells) and reduce the frequency and activity of immunosuppressive cells. This may increase the overall effectiveness and success of Nivolumab treatment. This pilot clinical trial will demonstrate whether combinatorial immunotherapeutic approaches that target epigenetic immune repression and RIG-I activity can favorably alter the tumor immune cell microenvironment and benefit patients with mucosal melanoma. For more information, please directly contact the CU melanoma clinic at (720) 848-0505.Opens in a new window Full story -
Center for Rare Melanomas Co-Hosts AIM Symposium for Rare MelanomasOpens in a new window
Sep 25, 2022The CU Center for Rare Melanomas and the CU Cancer Center co-hosted the hybrid "Living With Melanoma Patient Symposium: Rare Melanoma" on September 24, 2022 at the CU Anschutz Medical Campus. This symposium included presentations by clinicians, researchers, and patients focused on rare melanoma subtypes including uveal, mucosal, and acral melanomas. The presentations were recorded and you can watch them by following the link for this article!Opens in a new window Full story -

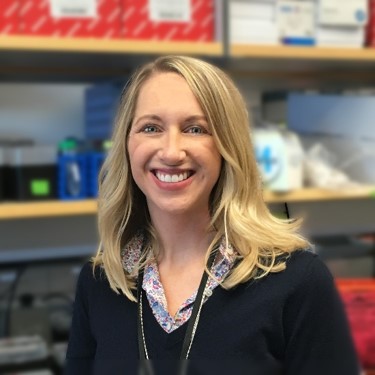
Kasey Couts, PhD, Recipient of Melanoma Research Alliance Young Investigator AwardOpens in a new window
May 11, 2022Kasey Couts, PhD, has been awarded the Melanoma Research Alliance Young Investigator Award "Women in Melanoma" for her research: Targeting anti-tumor immunity in anatomically distinct mucosal melanomas. Dr. Couts is an Assistant Professor of Research in the Division of Medical Oncology. Additionally, she serves as co-director for the CU Center for Rare Melanomas where she and her co-director Bill Robinson, MD, PhD, aim to build a comprehensive clinical and research center dedicated to understanding and treating rare melanomas. Rare types of melanomas including acral, mucosal, and ocular are considered melanomas but are very different diseases that remain not well understood resulting in less effective treatments for patients with these rare disease types. Mucosal melanomas have poor anti-tumor immunity compared to cutaneous melanomas with preliminary data showing widespread epigenetic silencing of innate immunity and other critical immune-related genes in mucosal melanoma. Dr. Couts hopes to provide insight as to how this relates to anti-tumor immunity and response to immune checkpoint inhibition, which still remains unclear. Congratulations Dr. Couts!Opens in a new window Full story -

CU Cancer Center Members Receive Grants to Conduct High-Tech ResearchOpens in a new window
Feb 10, 2022The Tumor-Host Interactions Program (THI) at the University of Colorado Cancer Center has awarded four CU Cancer Center researchers $30,000 each to gain preliminary data using the Multiplex Ion Beam Imager (MIBI) housed in the cancer center’s Human Immune Monitoring Shared Resource (HIMSR) to support a competitive national grant proposal. The selected researchers are expected to submit a national competitive grant proposal within six months of completing their THI-MIBI pilot studies.Opens in a new window Full story -

Presenting rare melanoma research at the 2019 International Congress of the Society for Melanoma Research
Nov 20, 2019 byThis year’s annual meeting of the Society for Melanoma Research (SMR) will take place from November 20-23 in Salt Lake City, UT. Once again, SMR has designated a special session of the Congress specifically to rare melanomas. Dr. Kasey Couts will be presenting her research on mucosal melanoma immune responses in this session. Other research personnel, including Robert Van Gulick and Morgan MacBeth, will be presenting posters on their research involving rare melanomas including a summary of the biorepository’s rare melanoma models and the identification of a new BRAF gene splice variant in ocular melanoma. You can follow highlights from this year’s meeting on SMR’s twitter account (@SocietyMelanoma).Full story -

Establishment of the CU Center for Rare Melanomas
Nov 20, 2019 byWhen you think of melanoma, you picture the sun. But there is another rare class of these dangerous melanomas that has nothing to do with sun exposure. Building on a unique expertise developed while researching and treating Colorado’s mile-high rate of sun-associated melanoma, University of Colorado Cancer Center recently earned designation as a Center for Rare Melanomas. The Center was established from a $1.5M award from the Patten Davis Foundation, and will help the team capture data from their clinical efforts that will aid in creating new understanding of, and new treatments, for the condition.Full story -

New “Rare Melanomas” session introduced at the 2018 International Congress of the Society for Melanoma Research
Oct 24, 2018 byThe Society for Melanoma Research (SMR) hosts an annual International Congress where researchers from around the world share their cutting edge work in melanoma. For the first time this year, the Congress has designated a special session focused specifically on rare melanomas. Dr. Kasey Couts is one of five speakers invited to share her research during this inaugural session. She will present the results of a collaboration with Foundation Medicine, Inc., a clinical testing company, which analyzed the genomics of rare melanomas and identified new targeted therapies that are effective in rare melanoma pre-clinical models and patients.Full story -
Lung cancer driver ALK-fusion found in melanoma
Oct 23, 2017 byA University of Colorado Cancer Center study published in the journal Molecular Cancer Therapeutics may offer hope to some of patients with melanomas caused by genetic changes not related to sun exposure. The study finds a genetic change called ALK-fusion in a patient sample of a melanoma subtype called mucosal melanoma. When researchers treated a tumor grown from this sample with the drugs crizotinib and ceritinib – both FDA approved to treat ALK-positive lung cancer – the tumor responded dramatically.Full story -

Scientists present rare melanoma research at the 2017 International Pigment Cell Conference.
Aug 26, 2017 byThis year’s International Pigment Cell Conference (IPCC) is being held in Denver, CO, from August 26-30. Topics at the annual IPCC meetings cover a wide variety of skin-related research topics, including basic skin cell functions, skin disorders, and cancers of the skin including melanoma. Two researchers from the CU Anschutz Medical Campus, Dr. Kasey Couts and Dr. Jennifer Hintzsche, will be presenting their research on rare, non-sun exposed melanomas.Full story -
New driver, target in advanced mucosal melanoma
Mar 15, 2017 byWhile most melanomas appear on the skin as the result of sun exposure, a small subset of melanomas arise spontaneously from mucosal tissues. A University of Colorado Cancer Center study published in the journal Melanoma Research demonstrates novel mutations involved in mucosal melanoma, paving the way for therapies to treat this overlooked subtype.Full story