OSSEOINTEGRATION
Advanced reconstructive surgery technique for amputees
What is Osseointegration?

Osseointegration is an advanced reconstructive surgery technique for amputees that eliminates the need for a traditional prosthesis. Because the implant connects directly with the bone of the residual limb, osseointegration patients regain body awareness and improve their balance and gait.
Osseointegration offers patients a better quality of life and improved function & mobility without the usual socket prosthesis-related issues such as pinching, sweating, muscle weakness, and skin irritation.
Osseointegrated bone-anchored prostheses can be implanted in the humerus (upper arm bone), radius or ulna (forearm bones), femur (thigh bone), or tibia (lower leg bone).
How Does Osseointegration Surgery Work?
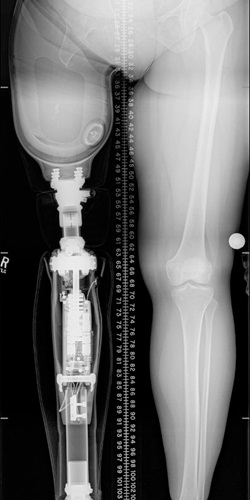
Osseointegration surgery is done in 1 or 2 stages depending on the implant type, design, and individual patient needs. First, a titanium implant is placed into the bone of the residual limb. The implant then extends through the skin and allows for a direct connection to a prosthesis. While healing, the arm or leg implant becomes unified with the bone, which allows the prosthetic limb to act more like a direct extension of the residual limb.
There are two types of osseointegration techniques: screw-fit (OPRA) and press-fit. Press-fit implants are typically done in a single-stage technique and can be performed on multiple locations of the body. Screw-fit (OPRA) implants are only available for transfemoral amputations and are done in a two-stage technique. The Limb Restoration Program offers both types of implants, depending on which technique is most appropriate for the patient’s needs and insurance coverages.
What are the advantages of Osseointegration surgery?
Increased Body Awareness
Ambulating (walking) with the connected prosthesis provides direct feedback to and through the skeleton creating greater balance, proprioception (sensing the position and movement of the body), and osseoperception (knowing and feeling where the bones are without looking).
This increased proprioception allows for improved balance and body awareness, and bony receptors generate an appreciation for texture and ground angle when walking and driving.
Improved Gait and Mobility
With increased body awareness, patients gain a more natural gait (way of walking). Osseointegrated prosthetics allow for a greater range of motion and allow for better bone and muscle mass growth. Patients experience stronger limbs which lets them lead a more active life. The prosthesis connected to the osseointegrated arm or leg implant takes seconds to clip on or off, leaving patients more time living and less time gearing up.
Reduces Pain
Socket-fit prosthetics typically cause patients to experience pinching, sweating, skin irritation, sores, ulcers, and nerve pain (neuroma). Nerve pain can also take the form of phantom limb pain. Socket prostheses put pressure on the nerves in the residual limb, which increases pain. Bone-anchored prosthetics reduce much of this pain because there is no socket prosthetic for the residual limb to press against.
Eliminates Poor Fit Issues
Because each body is unique, finding a prosthesis that fits a particular patient’s body can be difficult, especially when the size of the residual limb fluctuates during the first 12-18 months after amputation surgery. This leads to repeat visits with to a doctor or prosthetist to correct the issue, and can even lead to falls or further injury.
Each of our bone-anchored prostheses is custom-made, so they work with the patient’s body as is. Bone-anchored prosthetics also eliminate the excessive sweating, chafing, or skin issues amputees experience with traditional socket limb prosthetics.

Restores Freedom and Confidence
Reduced pain and increased mobility mean leading a fuller life. Our patients report an increase in meaningful activities and a dramatic decrease in prosthetic-related anxiety, such as:
- Worrying about where to park their car
- How long it takes to get up to go to the bathroom in the middle of the night
- Being able to sit comfortably on a chair or toilet
- Worrying about their ability to walk more than a short distance
- Sitting for long periods of time when traveling
- Walking on uneven ground, such as grass or dirt
Specialized types of prosthetic limbs, like those for showering or swimming, can be directly connected to the osseointegrated limb.

Who is a candidate for Osseointegration implants?
Osseointegration implants are a good option for amputees who are having a poor experience with their current prosthesis or do not want to use a traditional prosthetic leg or arm. Socket prostheses can be difficult for patients with a residual limb that is scarred, short, or wide. Because osseointegrated implants are implanted directly into the remaining bone, the shape of the residual limb does not cause the pain and discomfort patients typically feel with a traditional socket prosthesis.
If you are interested in becoming a candidate for osseointegration surgery with the CU Limb Restoration Team, you can begin the process by filling out the Osseointegration Pre-Screening Questionnaire and returning it to our clinic.
Why choose the University of Colorado Limb Restoration Program?

Dr. Jason Stoneback, Director of the Limb Restoration Program, is one of the few physicians across the globe that has been trained in all osseointegration implant procedures.
Since its founding in 2015, the University of Colorado Limb Restoration Program has been unique in its comprehensive, multidisciplinary approach. All of our patients receive world-class care and personalized attention. Each patient is monitored by our Osseointegration Program Coordinator, who guides patients through the program. Our team includes a social worker and amputee rehabilitation specialist, as well as physicians specializing in wound care, plastic surgery, foot & ankle care, interventional radiology, endocrinology, rehabilitation medicine, prosthetics, infectious disease, gait analysis, vascular medicine, and musculoskeletal oncology. We are proud to earn our 100% patient satisfaction rate.
Learn more about the CU Limb Restoration Team.