University of Colorado Limb Restoration Program
The University of Colorado Limb Restoration Program is a one-of-a-kind medical specialty group based in Colorado, USA that provides comprehensive orthopedic, vascular, wound, and rehabilitative care to serve a growing number of patients with complex extremity injuries. Our program is the first of its kind to deliver holistic, patient-centered care to people living with limb loss or who are at risk of losing a limb.
The interdisciplinary collaboration of more than 20 expert specialists combined with state-of-the-art treatment options allows our team to diagnose and treat the most challenging cases. We offer innovative treatment options to help avoid amputation where possible and to restore function and quality of life.
Conditions We Treat
- Bone Malunions and Nonunions
- Limbs needing Amputation
- Osseointegration Surgery in Amputees
- Bone or Limb Deformities
- Congenital Bone and Limb Conditions
- Limbs of Different Lengths
- Limb Difference
- Genu Varum
- Genu Valgus
- Bone and Soft Tissue Tumors
- Osteomyelitis
- Skeletal Dysplasias
- Chronic Wounds and Wounds Requiring Free Flap Coverage
- Peripheral Nerve/Brachial Plexus Surgery
- Vascular Diseases Putting Extremities at Risk
- Severe Traumatic Injuries
- Tarsal Tunnel Syndrome
- Stature Correction
- Bone Transport Surgery
If you are experiencing one of the conditions above or another that affects your limbs or has caused you limb loss, please contact our Limb Restoration Nurse Navigator to discuss your health.
Why Choose the University of Colorado Limb Restoration Program?
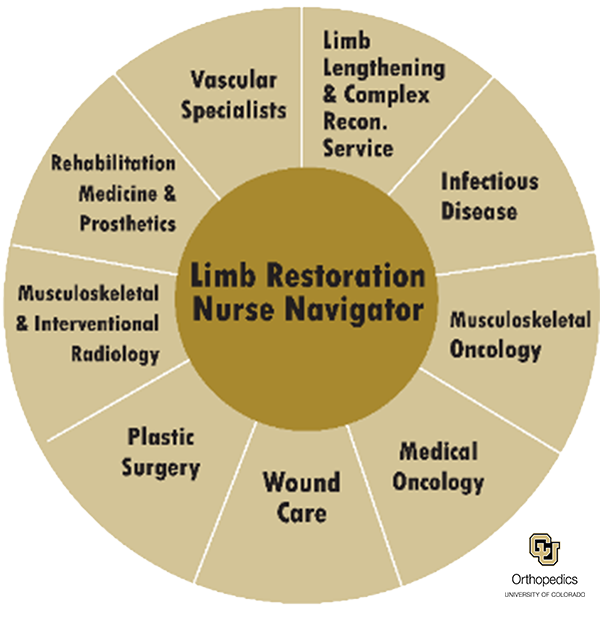
Unmatched, multidisciplinary care team
Since its creation in 2015, the University of Colorado Limb Restoration Program has been unique in its comprehensive, multidisciplinary approach. With the dedicated attention of our Nurse Navigator to facilitate communication and timely treatment, the CU Limb Restoration Program can combine the talents of many specialists and sub-specialists located at the UCHealth Anschutz Campus. This includes doctors from more than 10 specialties, advanced practice practitioners, a social worker, administrative support, and more. Our team meets every week to review and consult on all our cases, ensuring the best treatment plan for each patient. But the most important member of your limb restoration healthcare team is you. After you leave our campus in Colorado, we continue to communicate and collaborate with you and your local care team to ensure your safe transition back to your community.
Our team includes specialists in the fields of:
- Orthopedics
- Wound Care
- Plastic Surgery
- Foot & Ankle Care
- Interventional Radiology
- Endocrinology
- Rehabilitation Medicine
- Prosthetics and Orthotics
- Infectious Disease
- Gait Analysis
- Vascular Medicine
- Musculoskeletal Oncology
Patient Reviews

Dr. Jason W. Stoneback, Director of the Limb Restoration Program, specializes in the treatment of simple and complex fractures, non-unions, malunions, osteomyelitis, orthopedic infections, limb-length discrepancies, deformity correction, post-traumatic limb salvage and novel osseointegration surgery in amputees. Dr. Stoneback was one of the first orthopedic surgeons to offer osseointegration surgery in the United States and is widely considered to be one of the best American osseointegration surgeons. He strongly believes in the connection between form and function and strives to provide patients with real options – often when all other choices have been exhausted.
Learn more about Dr. Stoneback’s clinical and research work by clicking here
Clinic Location - Telehealth available across the country
Our clinic is located in UCHealth’s Anschutz Outpatient Pavilion in Aurora, Colorado, but we offer telehealth in many states across the United States. Dr. Jason Stoneback is licensed in Wyoming and Colorado, and Dr. Danielle Melton is licensed in Arizona, Colorado, Idaho, Kansas, Mississippi, Montana, Nebraska, Nevada, Oklahoma, South Dakota, Texas, Utah, Washington, and Wyoming. After your treatment in Colorado, we will be able to follow up with you every step of the way.
Practice Location
CU Limb Restoration Program - University of Colorado Hospital
1635 Aurora Court Anschutz Outpatient Pavilion, 4th floor,Aurora, CO 80045
To make an appointment call:
Phone: 1-844-800-LIMB (5462)
Fax: 720-553-0402
E-Mail: [email protected]
For urgent or emergency transfers, call the Access Center at:
Phone: (720) 848-2828
For more information on how to contact us or send us a referral, please click here.
Limb Restoration News
-
Restored Limb Puts Cyclist Back in the RaceOpens in a new window
Oct 15, 2025The University of Colorado Anschutz is a world-class academic medical campus at the forefront of transformative science, medicine, education and patient care. The campus encompasses the University of Colorado health professional schools, more than 60 centers and institutes and two nationally ranked independent hospitals - UCHealth University of Colorado Hospital and Children's Hospital Colorado – which see more than two million adult and pediatric patient visits yearly. Innovative, interconnected and highly collaborative, CU Anschutz delivers life-changing treatments, patient care and professional training and conducts world-renowned research.Opens in a new window Full story -
Osseointegration: Nuts and Bolts of OIOpens in a new window
Jan 13, 2026Join leading experts from the University of Colorado Limb Restoration Program—Dr. Jason Stoneback and Dr. Danielle Melton—as they share the latest insights, advancements, and practical knowledge in the field of osseointegration.Opens in a new window Full story -

At the Forefront” Chancellor Newsletter, “Love, Life and Limbs Restored
Feb 13, 2024For Josh and Melissa Bryan, it was love at first sight. Though these high school sweethearts parted ways when Melissa went to college, they rekindled their relationship five years later at a family wedding.Full story -

Bone-anchored Prosthesis Doesn’t Prevent Limb-loading AsymmetryOpens in a new window
Jun 14, 2024While early evidence suggests improvement in joint and limb loading mechanics during walking with a bone-anchored limb compared to socket prosthesis use, a team of researchers foundOpens in a new window Full story