Post-Operative Information
What to Expect After Surgery
- Diet after surgery: Resume your diet gradually. Begin with clear liquids and gradually progress as you feel ready.
 Surgical Site Care: Please remain in your post-operative dressing/splint until your first post op appointment with Sikora Cain PA-C or Dr. Moon. Please
make sure to keep your post-operative dressing clean and dry. Please use a shower bag (e.g., www.drycast.com) when showering or bathing to keep things dry. Wet padding can cause skin
breakdown.
Surgical Site Care: Please remain in your post-operative dressing/splint until your first post op appointment with Sikora Cain PA-C or Dr. Moon. Please
make sure to keep your post-operative dressing clean and dry. Please use a shower bag (e.g., www.drycast.com) when showering or bathing to keep things dry. Wet padding can cause skin
breakdown.
- Do not stick anything down your cast or splint. If you sustain a scratch, you are at higher risk for infection as casts and splints harbor more bacteria.
- Follow Up Appointment: Please call the CU Orthopedic Surgery clinics (Longmont, Boulder, or Central Park) or Dr. Moon's schedulers within two (2) days of your discharge to /confirm/verify your follow-up appointment date/time with Dr. Moon or Sikora Cain, PA-C. Typically, we will want to see you 14-21 days after surgery for a post-operative follow-up appointment - before 14 days, the sutures may have to stay in and you will need to return in the 14-21 day window again. Please arrive ~15 minutes prior to your appointment time to take care of any paperwork.
Activity Precautions
 Elevate the leg above your heart as much as possible
for at least the first two weeks after surgery, until your first follow-up visit. If the leg is higher than your heart, gravity helps decrease swelling, decrease pain, and improve blood flow. If the leg is below your
heart, swelling increases, pain can worsen, and your wound is at greater risk of infection.
Elevate the leg above your heart as much as possible
for at least the first two weeks after surgery, until your first follow-up visit. If the leg is higher than your heart, gravity helps decrease swelling, decrease pain, and improve blood flow. If the leg is below your
heart, swelling increases, pain can worsen, and your wound is at greater risk of infection.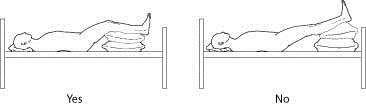
- Keep all weight off of your surgical leg until cleared by your physician.
- You will be non-weight-bearing on your surgical lower extremity even if you are discharged from surgery wearing a CAM boot or postop shoe.
- Use ice packs intermittently (20 minutes on, 20 minutes off) to reduce pain and swelling, however, use extreme caution with icing if your block is still in effect. Make sure to have a barrier between your skin and the ice pack to avoid frostbite.
- If you are in a post-operative splint, you can wiggle your toes to help push swelling to your lymph ducts, but do not try to move your ankle.
Pain Management
- Nerve Blocks: to help control pain after surgery, you may receive a nerve block where the anesthesiologist injects numbing medication around the nerves that send pain signals from your foot or ankle to your brain. This helps you feel little to no pain.
- The time a nerve block lasts varies from person to person. Often they will last between 12 and 24 hours but could last days. You may not be able to move your foot and/or ankle during this time.
- As the block medication wears off, you may feel a tingling sensation as the nerves start to wake up.
- Keep your foot and ankle safe while it is numb. Avoid excessive heating, scratching, etc. until the block has completely worn off.
- If icing the ankle or foot, watch the toes closely to ensure that they do not become discolored (i.e., white, red or blue)
- Even if you still feel no pain in your leg before you go to bed, take a dose of your narcotic medication before you go to sleep. You do not want to wake up with the block has worn off and being behind on pain control - it is quite difficult to 'catch up' again.
- Pain Medication:
- Acetaminophen (Tylenol) 500mg tablets are typically your baseline pain medication. Take this tablet up to once every 4 hours. Do not exceed 3,000mg of acetaminophen daily.
- You may be provided narcotic pain medication as your initial pain reliever. Take doses of this medication if you are having severe breakthrough pain uncontrolled by the Tylenol alone. Typically, patients are taking it every 4 hours for the first day or two after surgery. Actively wean down your use of this medication after the third day after surgery.
- DO NOT drink alcoholic beverages, use recreational drugs, or use prescription sedative medications when taking pain medication.
- DO NOT operate heavy machinery/drive while taking opioids.
- To avoid the risk of nausea, please make sure that you are taking your medication with food.
- You may experience lightheadedness while taking your pain medication.
- Make sure you drink plenty of water while taking narcotic pain medication to stay well hydrated and help avoid constipation.
- You may be provided a Senokot-S prescription to help with constipation which can be a side effect of taking narcotics. Take that medication as needed.
- You may be provided a Hydroxyzine prescription to help with nausea that you can take as needed.
- Itching is a common side effect of pain medication usage. If you have an associated rash with the itching, please contact your provider. Hydroxyzine or OTC Benadryl can be used to help with itching.
When to Call Your Physician
- Common or normal post-operative reactions:
- Low-grade fever (approximately 100.5 degrees) for up to one week.
- A small amount of blood or fluid leaking from the surgical site or dressing
- Bruising along the surgical extremity
- Swelling around the surgical site and surrounding area
The reactions listed above are NORMAL, but you want to call your surgeon if any of these reactions persist.
- Symptoms to report:
- Please report any of the following signs to your surgeon:
- Signs of infection:
- Redness or pain around your incision (if you cannot see your incision, red streaking up your extremity should be reported).
- Thick, dark yellow, or foul-smelling drainage at the incision site or from your dressing.
- Temperature measured over 101.5 degrees for more than 24 hours despite Tylenol.
- Signs of Decreased Circulation to the Ankle and Foot:
- Coldness of ankle and foot
- Foot or leg turning pale
- Tingling/numbness (after the block has fully resolved)
- Sustained increases in pain uncontrolled by medication
- Toenail bed turns blue in color
- Blood Clots: Although rare, please be aware and utilize the recommendations below to avoid getting a blood clot.
- Prevention of deep vein thrombus DVT (blood clots):
- You may be provided a prescription for daily Aspirin or other anticoagulant medication to help prevent blood clot formation.
- Get up 4-5 times during the daytime and walk/crutch/walker across the room to keep the blood circulating in your legs. (Maintain any weight-bearing restrictions, of course)
- Wiggle your toes frequently if you are in a splint or cast
- Notify your physician if you are a nicotine user, on hormone replacement therapy medications, are taking birth control, or have a history of blood clots as these can increase your risk of developing a blood clot.
- Notify your provider if you develop pain or tenderness in your calf muscle
If you have any additional questions, please contact Dr. Moon's staff at the following phone numbers:
- CU Medicine Orthopedics Longmont Clinic: 720-718-8288
- UCHealth Foot and Ankle Center (Central Park - Denver): 720-848-3668
- CU Sports Medicine and Performance Center (Boulder): 303-315-9900
IF YOU HAVE AN EMERGENCY, i.e., SHORTNESS OF BREATH, CHEST PAIN, OR SYMPTOMS SEVERE IN NATURE, PLEASE CALL 911 OR VISIT YOUR LOCAL EMERGENCY ROOM

