Treatment of Ankle Fractures
Ankle Fracture
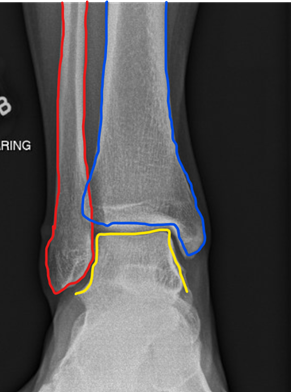
The ankle joint is comprised of three bones: the tibia, fibula, and talus which articulate together. The ends of the fibula and tibia (lower leg bones) form the inner and outer malleolus, which are the bony protrusions of the ankle joint that you can feel and see on either side of the ankle. The joint is protected by a fibrous membrane called a joint capsule, which is filled with synovial fluid to enable smooth movement.
Ankle injuries are common in athletes and patients engaged in physical work, often resulting in severe pain and impaired mobility. Pain associated with ankle injuries may be the result of a torn ligament (“sprain”) or a broken bone (“fracture”). An ankle fracture is a painful condition involving a break in one or more bones forming the ankle joint. The ankle joint is stabilized by different ligaments and other soft tissues, which may also be injured when an ankle fracture is suffered. In severe cases, the fracture may result in one of the ankle bones piercing and protruding through the skin. This is called an open fracture and typically requires multiple surgeries.
Causes
Ankle fractures usually result from trauma or excessive rolling and twisting of the ankle, which are generally caused by a specific accident or a variety of physical activities such as jumping or falling that places stress on the joint.
Symptoms
Ankle fractures, generally result in immediate swelling and pain around the ankle as well as impaired mobility. In some cases, blood may accumulate around the damaged joint, a condition called hemarthrosis. Additionally, bruising and redness occur at the ankle and foot and sometimes fracture blisters appear in severe cases.
Types of Fractures
Ankle fractures are classified according to the location and type of ankle bone involved. The different types of ankle fractures are generally classified as follows:
- Lateral Malleolus fracture - the lateral malleolus, or outer part of the ankle, is fractured.
- Medial Malleolus fracture - the medial malleolus, or inner part of the ankle, is fractured.
- Posterior Malleolus fracture - the posterior malleolus, or bony hump of the tibia, is fractured.
- Bimalleolar fracture - both lateral and medial malleolus bones are fractured.
- Trimalleolar fractures – the lateral, medial, and posterior malleolus bones are all fractured.
- Syndesmotic injury - also called a high ankle sprain, is generally not considered a fracture but may be treated as a fracture since it causes ankle instability and long-term complications.
Diagnosis
Diagnosis of an ankle injury begins with a physical examination and is usually followed by an X-ray and possibly a CT scan for a more detailed view. Without a radiologic study such as an x-ray or CT scan, it may be difficult to differentiate a broken ankle bone from other conditions such as a sprain, dislocation, or tendon injury. Depending on the nature of the injury, the physical examination may include a “stress test” which evaluates the stability of a suspected ankle fracture, which, in turn, may determine whether surgery is necessary. In complex cases, a detailed evaluation of supporting ligaments through an MRI scan may be recommended.
Treatments
Immediately following an ankle injury (and prior to seeing a provider), patients should apply ice packs and keep their injured ankle elevated, to minimize pain and swelling.
Treatment of an ankle fracture usually depends on both the type and stability of the fractured bone. Treatment usually begins with non-surgical methods, in order to decrease soft tissue swelling. However, in cases where the fracture is unstable and/or cannot be realigned, surgical treatment may be required right away.

 With non-surgical treatment, the ankle bone is realigned, and a plaster splint is placed around the joint, for at least 2-3 weeks.
With surgical treatment, the fractured bone is usually accessed by making an incision over the ankle and then the broken pieces are aligned and compressed together. The bones are fixated with screws and usually, a metal plate is then placed on top for
added protection and support. The incision is then sutured closed, and the ankle is immobilized with a splint.
With non-surgical treatment, the ankle bone is realigned, and a plaster splint is placed around the joint, for at least 2-3 weeks.
With surgical treatment, the fractured bone is usually accessed by making an incision over the ankle and then the broken pieces are aligned and compressed together. The bones are fixated with screws and usually, a metal plate is then placed on top for
added protection and support. The incision is then sutured closed, and the ankle is immobilized with a splint.
Post-Operative Care
After ankle surgery, patients are instructed to avoid placing weight on the ankle by using crutches, a walker, and/or a knee scooter for at least six weeks.
Physical therapy is usually necessary to rehabilitate the ankle after surgery. After 2-3 months of physical therapy, the patient may be able to perform normal daily activities. High-impact activities can usually be resumed 6 months post-operatively.
Risks and Complications
Some of the risks and complications associated with ankle fractures include decreased ankle range of motion/stiffness, chronic pain, ankle arthritis, wound complications, infection, and/or nerve damage resulting in pain.
Although not usual, surgery may result in incomplete healing of the fracture, which could require subsequent revision surgery to repair. This risk/complication is more common in patients who use nicotine products and those with uncontrolled diabetes.

