Racial and Ethnic Disparities in the Delayed Diagnosis of Appendicitis Among Children
A PECARN Registry study co-authored by Dr. Lalit Bajaj
Marion Ruth Sills, MD, MPH | Department of Pediatrics, School of Medicine Nov 22, 2020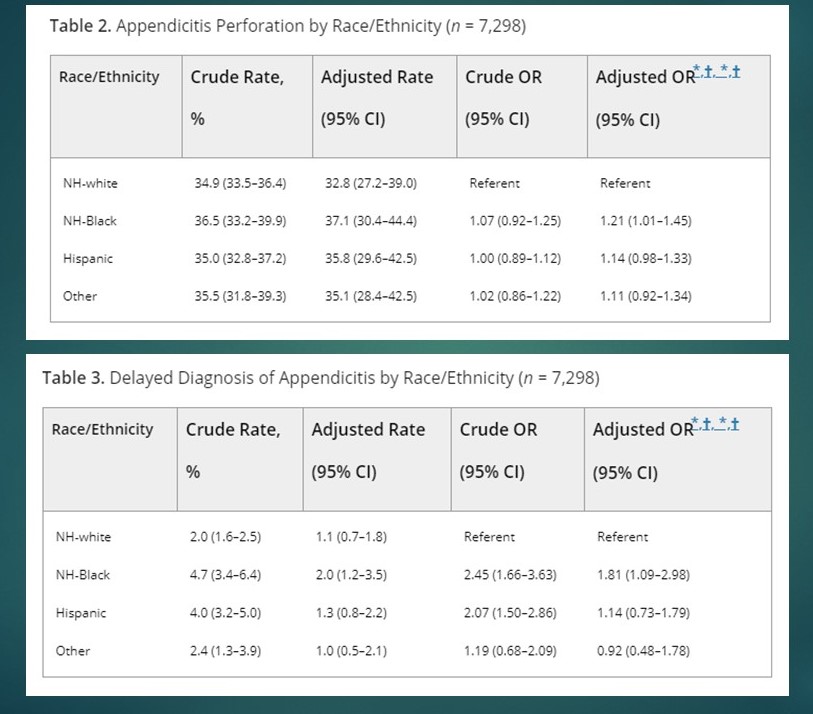
A Pediatric Emergency Care Applied Research Network (PECARN) Registry study co-authored by pediatric emergency physician Lalit Bajaj found racial disparities in rates of delayed diagnosis of appendicitis and diagnostic imaging during prior emergency department (ED) visits.
In a study involving 7,298 children diagnosed with appendicitis at seven EDs, non-Hispanic Black children had higher rates of appendiceal perforation (36.5%; aOR = 1.21 [95% CI = 1.01 to 1.45]) than did non-Hispanic white children (34.9%). Odds ratio calculations were adjusted for age, sex, insurance, site type, senior provider level, triage category, and highest pain score during initial visit and site.
Non-Hispanic Black children had higher rates of delayed diagnosis of appendicitis, defined as having a delayed diagnosis of appendicitis if they had a prior ED visit for a related complaint in the 7 days preceding appendicitis diagnosis. In comparison to non-Hispanic whites (2.0%), non-Hispanic Black children had higher rates of delayed diagnosis of appendicitis (4.7%; aOR = 1.81 [95% CI = 1.09 to 2.98]).
Non-Hispanic Black children were less likely to undergo definitive imaging (CT, MRI, and/or US) during prior ED visit(s) when compared to non-Hispanic white children. Of the 206 children with a delayed diagnosis of appendicitis, 89 (43.2%) had some form of diagnostic imaging during their prior ED visit(s). In comparison to non-Hispanic white children (46.2%), non-Hispanic Black children had lower rates of diagnostic imaging (28.2%; aOR = 0.41 [95% CI = 0.18 to 0.96]).
These results suggest that when children present to the ED with symptoms that may be consistent with appendicitis, patients are differentially managed based on their race/ethnicity. This differential management may, in part, contribute to higher rates of appendicitis perforation among minority children.