Our City
300 days of sunshine
At the foot of the Rocky Mountains, Denver is known for sweeping views and a wide array of outdoor activities
Overview
Our fellowship program provides comprehensive training in the subspecialty of Pediatric Emergency Medicine (PEM). Graduates learn to independently manage all medical conditions that would fall under the purview of a Pediatric Emergency Medicine subspecialist.
Learning from direct patient care is augmented by numerous integrated longitudinal curricula involving research, critical appraisal of literature, quality, toxicology, simulation, EMS/transport, DHEI, self-directed and facilitated educational activities. Our fellows are required to participate in quality projects, lead a scholarship project, produce a first-authored manuscript, and provide education to a variety of trainees, faculty, and medical professionals throughout their fellowship.
Fellows rotate primarily through Children’s Hospital Colorado (Children's Colorado) located on the Anschutz Medical Campus in Aurora, Colorado. Children's Colorado is the only free-standing, quaternary care pediatric hospital in Colorado and the only Level 1 Regional Pediatric Trauma and Burn Center in the state with regional referrals from the surrounding 7-state region.
Program Aims
Meet the Fellows... | Tour Children's Hospital Colorado... |
Our City
300 days of sunshine
At the foot of the Rocky Mountains, Denver is known for sweeping views and a wide array of outdoor activitiesOur Hospital
Ranked No. 1 in the Rocky Mountain Region
Children’s Hospital Colorado consistently ranks in the top 20 on the U.S. News Best Children’s Hospitals Honor Roll
Our Section
180,000+ Visits Annually
Our large and diverse faculty care for patients presenting with a broad array of conditions
Clinical Training
The primary focus of our clinical training is to provide comprehensive training in Pediatric Emergency Medicine (PEM) to allow the graduate to independently manage acutely ill and injured children.

Fellows are directly supervised by Pediatric Emergency Medicine and Emergency Medicine faculty during their clinical ED rotations. Under the supervision of a large and diverse faculty, trainees gain exposure to patients with a broad spectrum of clinical conditions. To prepare trainees to function as effective Pediatric Emergency Medicine subspecialists upon completion of their fellowship, the fellows assume graduated responsibility for patient care over the course of three years.
First Year
During their first year, fellows function as direct care providers, focusing on honing clinical and procedural skills. In the second half of the year, fellows will have shifts in which they provide clinical supervision of junior trainees and learn ED management/flow under the direct supervision of a PEM attending.
The first year for pediatric-trained fellows includes:
For emergency medicine-trained fellows:
Second Year
During the 2nd half of their second year, fellows begin the transition from caring for patients directly to becoming the supervising physician in charge of an ED team. In their second year, the total amount of clinical time decreases compared to year I and fellows assume more teaching and supervisory responsibilities and dedicate more time to scholarship projects. As part of their clinical requirement, fellows begin “Pre-tending” or “Attending” Shifts where they gradually assume the responsibilities of the Attending ED physician under direct supervision.
The second year for pediatric-trained fellows includes:
For emergency medicine-trained fellows, clinical responsibilities during Year 2 transition to 3rd year fellow expectations of Pediatric-trained fellows.
Third Year
During their third year, fellows become proficient in running a large, urban, Level 1 Trauma Pediatric ED. Fellows take primary responsibility for patients, trainees, and other providers on the ED team, referral and transfer calls, and are expected to maintain an effective working relationship and communication with the charge nurse, nursing and ancillary staff.
The third year for pediatric-trained fellows includes:
Sample Block Schedule for Pediatric Residency Graduates:
| 1st Yr Rotation | # Clinical ED Shifts |
| 1st Yr Rotation | # Clinical ED Shifts |
|---|---|
| Adult ED (1 month) | 12 |
| Pediatric Critical Care (1 month) | 0 |
| Peds Anesthesia (1 month) | 4 |
| Toxicology (1 month) | 6 |
| Research (1 month) | 8 |
| PEM ED shifts (6 months) (Includes 2-week Ultrasound Block) | 90-100 |
| Totals | 108-118 PEM ED Shifts 12 Adult ED Shifts |
| 2nd Yr Rotation | # Clinical ED Shifts |
| 2nd Yr Rotation | # Clinical ED Shifts |
|---|---|
| Adult ED | 12 |
| EMS/Transport | 2-6 |
| Research (6 months) | 40-48 |
| PEM ED (2 months) | 28-32 |
| Electives | 3-6 |
| Attending shifts (2nd semester) | 18 |
| Totals | 100-110 PEM ED Shifts 12 Adult ED Shifts |
| 3rd Yr Rotation | # Clinical ED Shifts |
| 3rd Yr Rotation | # Clinical ED Shifts |
|---|---|
| Adult ED | 12 |
| Elective (1 month) | 0 |
| Adult ED POCUS (1 month) | 6 |
| Research (5 months) | 40 |
| PEM ED (4 months) | 48-58 |
| Totals | 88-98 PEM ED Shifts 18 Adult ED shifts |
Overview
The program provides comprehensive scholarly training that prepares all trainees with the background and skills to compete for academic faculty positions at the completion of their fellowship.
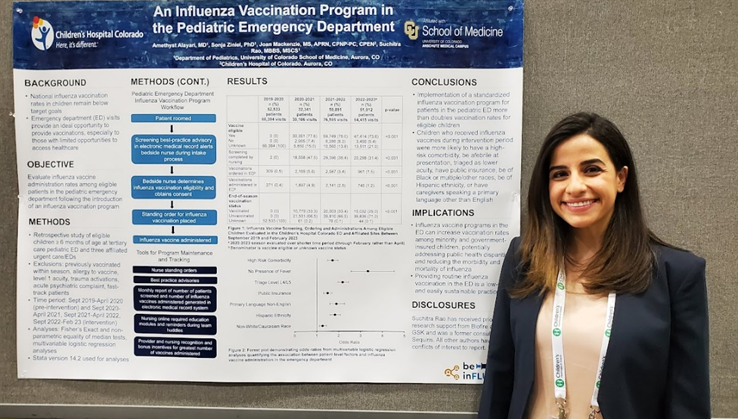
Graduates are expected to complete a scholarly project during their three years including presentation of the project at a national meeting, such as the American Academy of Pediatrics fall meeting or the Pediatric Academic Societies spring meeting, and submission of a first-authored manuscript to a peer-reviewed publication. Fellows are also required to be involved in QI.
Research Infrastructure
The Section has a full-time research coordinator and biostatistician who are available for assistance with study design, IRB applications, database management, statistical analysis, and grant submissions. Fellows have access to Professional Research Assistants (PRAs) who can assist with study enrollment and data collection in the Children’s ED. PRA coverage averages 10-16 hours per day.
Timeline for Pediatric-trained PEM fellows
PEM Fellowship Year 2:
PEM Fellowship Year 3:
*Emergency Medicine-trained PEM fellows have a 2- year curriculum. The scholarship project requirements are the same regardless of training path.
Scientific Meetings and Other Conferences
Pediatric Emergency Medicine fellows are encouraged to attend national scientific meetings throughout their fellowship. If funding is available, the Section supports travel to any national meeting for which the trainee has an abstract or platform presentation according to section guidelines.
National Research Networks
The University of Colorado Denver/Children's Colorado is a member of PECARN, the Pediatric Emergency Care Applied Research Network. PECARN is a federally funded pediatric emergency medicine research network conducting multi-institutional research on the prevention and management of acute illness and injuries in children and youth of all ages. For more information: http://www.pecarn.org/
Several faculty are members of PEM CRC, the PEM Collaborative Research Committee, a subcommittee of the American Academy of Pediatrics Section on Emergency Medicine. PEM CRC is an unfunded volunteer effort which provides a framework for multicenter investigation. It provides a means of developing protocols and identifying interested co-investigators at over 40 member sites. For more information: http://www.pemcrc.org/
Local Research Support
The Colorado Clinical and Translational Sciences Institute (CCTSI) is a collaborative enterprise between University of Colorado Denver, University of Colorado at Boulder, six affiliated Hospitals and health care organizations, and multiple community organizations with resources to promote research and training that will advance health care and improve the public health. Through the CCTSI, Clinical Translational Research Centers (CTRCs) have been established at several affiliated hospitals, including Children's Colorado, University of Colorado Hospital, and Denver Health Medical Center. The CTRC also offers biostatistical collaboration/consultation for study design, including sample size and power calculations, and data analysis. Children’s Hospital Research Institute also offered limited research support to fellows.
Overview
Learning from direct patient care is augmented by a comprehensive series of lectures and conferences focused on Pediatric Emergency Medicine and associated longitudinal curricula.

Specialty-Specific Curriculum
Fellows participate in several educational seminars focused on Pediatric Emergency Medicine. Most education takes place during mandatory sessions on Thursday that anchor the educational program.
Interactive Learning
Ultrasound Curriculum

Simulation Curriculum
Fellowship Tracks
New to our curriculum are optional fellowship tracks designed for those fellows who desire additional training with concentration in the following areas:
These tracks have specific mentored scholarship requirements, supplemental coursework, and educational/teaching responsibilities in addition to regular series fellowship curriculum requirements.
Fellow-Faculty Dinner Series

Quarterly dinners hosted by faculty to discuss specific topics such as career, wellness, and resiliency.
Additional Courses
Pediatric Biostatistics Course
Introductory six-session course in biostatistics given under the auspices of the Department of Pediatrics with the goal of developing familiarity with commonly used statistical methods and critically appraise literature.
Introductory Training Program in Quality Improvement
Fellows have the opportunity to apply for an 8-hour session by The Institute for Healthcare Quality, Safety and Efficiency (IHQSE) that covers the importance of quality science in health care, basic tools for analyzing processes of care and identifying opportunities for improvement, fundamental data collection and analysis techniques to support quality improvement projects, methods for creating and testing potential changes, and tactics for implementing and spreading improvement ideas.
Graduate Coursework
Masters of Science in Clinical Sciences (MSCS) program is offered through the university and select fellows through the Department of Pediatrics may apply for limited funding support for this program if grants are available. A mini-certificate or an MPH degree may be obtained at the Colorado School of Public Health (collaboration between University of Colorado Denver, Colorado State University and the University of Northern Colorado). For more information: www.publichealth.ucdenver.edu . The certificate program requires 15 hours of graduate work and the MPH requires 42 hours of graduate work. This requires extra time commitment as the clinical and elective requirements remain unchanged. Funding for trainee graduate coursework is not supported by the section of emergency medicine.
Additional Learning Opportunities:
Subspecialty Excellence in Educational Leadership & Scholarship (SEELS) Program :
Pediatric Fellowship Educational Series
This educational series has been developed by the Committee on Fellowship Education to address areas of scholarly interest common to all pediatric fellows. Nearly 100 sub-specialized physicians in training will attend 5-6 half-day seminars spread across their 3 years of fellowship.
Pediatric Biostatistics for Clinicians Course:
This course is primarily intended for 2nd and 3rd year Department of Pediatrics fellows as part of the comprehensive fellowship educational program. Designed to help fellows to develop an ability to be a critical consumer of the literature and develop familiarity with many commonly used statistical methods.
Advanced Degrees Available at CU:
*Indicates required teaching opportunity
Core Teaching Faculty
The section of pediatric emergency medicine has one of the largest PEM faculty groups in the country. These faculty have diverse interests & expertise, and are important contributors to fellows’ education, scholarship, and mentorship. Other clinical faculty also participate in fellowship education and training but are not listed below.
| Faculty Member | Research Interests | Education/Clinical Interests |
|---|---|---|
| Anna Abrams* Assistant Professor | Refugee Health, Health Disparities | |
| Kathleen Adelgais* Professor | EMS, Multisystem Trauma, Pediatric Pain Management | Prehospital/EMS, Regional EMS Engagement/Leadership |
| Chisom Agbim* Assistant Professor | Quality Improvement, Health Equity | Quality Improvement Curriculum |
| Lilliam Ambroggio* Associate Professor Director of Research Operations | Biomarkers, Respiratory Infections, Antimicrobial Stewardship | Fellows’ Research Curriculum Director |
| Lalit Bajaj Professor Director, Clinical Effectiveness | QI/Clinical Effectiveness, Bronchiolitis | |
| Julia Brant Assistant Professor | Ultrasound | |
| Cortney Braund Assistant Professor Medical Director, Anschutz ED | Operations | |
| Rachel Cafferty* Assistant Professor | Behavioral Health, Gender and Sexual Minority, SI Screening | -Pediatric agitation management for prehospital providers -Suicide care pathways for primary care, safety planning |
| Kevin Carney Associate Professor Associate Chief Medical Officer | Quality Improvement | Clinical Operations, Hospital Administration |
| Shannon Flood* Assistant Professor Director of Resident Simulation | Simulation Education | |
| Joe Grubenhoff* Associate Professor Medical Director of Diagnostic Safety | Diagnostic Safety | Cognitive Psychology of Clinical Decision-Making |
| Maya Haasz* Assistant Professor | Firearm Safety, Advocacy | Advocacy Curriculum Director for Peds Residency |
| Jon Higgins* Assistant Professor Assoc Director, Resident Education | Med Ed | Resident Education, Associate Director for Resident Pediatric ED Rotation |
| Bernadette “Bernie” Johnson Associate Professor Director of Clinical Operations | Operations | Clinical Operations |
| Kristin Kim* Assistant Professor | Trauma, Mass Casualty | Disaster Preparedness, Trauma Liaison |
| Andrew Krack* Assistant Professor | Airway management; HIKO-STEC study | Airway Management, Resuscitation; High Acuity/Low frequency events |
| Sam Lam Professor | Ultrasound | Ultrasound, General (adult) Emergency Medicine |
| Patrick Mahar* Associate Professor Resident Education Director | Mobile Simulation and Educational Outreach, Resident Education | |
| Maria Mandt Associate Professor Medical Director, Transport and EMS | Clinical Care Transport, EMS | Prehospital Transport and Program Administration |
| Nidhya Navanandan* Assistant Professor | Asthma | |
| Jon Osborn* Assistant Professor Director of Ultrasound | Point of Care Ultrasound in the ED | |
| Arleta Rewers* Professor | Acute Complications of Diabetes | |
| Mark Roback* Professor Section Head | Procedural Sedation Resuscitation Education | Section/Department/Hospital Administration Leadership and Career Development |
| Laura Rochford* Instructor Director of Resuscitation | Radiology Discrepancy, Resuscitation | |
| Kelley Roswell* Associate Professor Director, Medical Student Education | Medical Student Education, Educational Outreach | |
| Sarah Schmidt* Associate Professor Med Director Advanced, Informatics Assoc Med Director, Anschutz ED | Clinical Informatics | Clinical Operations, Informatics, Clinical Decision Support |
| Halden Scott* Associate Professor Director of Research, PEM | Sepsis, Resuscitation, Diagnosis, Pragmatic Trials | Sepsis |
| Sandra Spencer* Associate Professor Director of Faculty Academic Development | Quality Improvement | Quality Improvement, Faculty Development |
| Melisa Tanverdi* Assistant Professor | Asthma | |
| Irina Topoz* Associate Professor Director, Quality Improvement | Clinical Pathways, Quality Improvement, Patient Safety | Clinical Pathways, Quality Improvement, Patient Safety |
| Tien Vu* Associate Professor Program Director, PEM Fellowship | Post-Graduate Training & Competency, Med Ed, Administration | Fellowship Education |
| George “Sam” Wang* Associate Professor Faculty at RMPDS | Medical Toxicology | Fellowship Toxicology Curriculum, Phone Nurse Triage |
| Joseph Wathen* Associate Professor Director, Mass Casualty | Procedural Sedation, Disaster Training |


Alexandra Beatrice Berardi-Bloomfield, MD

Savannah Adelaide Zoe Brackman, MD

Erica K. Sheline, MD

Margaret Elizabeth Tashjian, MD

Tamara Burleson Garcia, MD, PhD

Kelsey Abigail Koff, MD

Erin Anne McGonagle, MD

Shelby Brooke Tanguay, MD

Amethyst Amy Alayari, MD

Daniel J. Lam, MD

Nithin Srinivasan Ravi, MD
| Academic Training Facility/Institution | Faculty (Private Community) | Continuing Education/ Fellowship | Military/Other |
|---|---|---|---|
| 82% | 7% | 7% | 4% |

All application material should be submitted through the Electronic Residency Application Service(ERAS) by August 2nd. Applications received after this date will not be considered due to the large number of applicants and short interview season. We participate in the National Residency Matching Program (NRMP) and typically do not offer any positions outside of the match. Required application materials include:
ERAS Application Timeline
| Date | Activity |
| Monday, May 31, 2024 | ERAS 2024 season ends at 5 p.m. ET. |
| Wednesday, June 5, 2024 | ERAS 2025 season begins at 9 a.m. ET. |
| Thursday, June 5, 2024 | EFDO will release tokens to fellowship applicants. |
| Wednesday, July 3, 2024 | July cycle fellowship applicants may begin submitting applications to programs at 9 a.m. ET. |
| Wednesday, July 17, 2024 | July cycle fellowship programs may begin reviewing applications at 9 a.m. ET. |
| May 31, 2025 | ERAS 2025 season ends at 5 p.m. ET |
NRMP Fall Match Timeline
| Dates | Activity |
| Wednesday, August 21, 2024 | Match Opens |
| Wednesday, September 25, 2024 | Ranking Opens |
| Wednesday, November 6, 2024 | Quota Change Deadline |
| Wednesday, November 20, 2024 | Rank Order List Certification Deadline |
| Wednesday, December 4, 2024 | MATCH DAY |
Applications
Applications will be accepted as soon as the ERAS opens to programs on July 19th, 2023. Applications must be submitted before August 2nd. Due to the large number of applicants, we will not be reviewing applications submitted after this time or applications which are significantly incomplete may not be considered. Additional dates for the Pediatric Emergency Medicine fellowship match are provided below.
Interviews
Our program will be conducting all-virtual interviews this season. Communications from the program will either come through ERAS or to the applicant’s designated email address. Applicants will be notified of their status by August 16th. The PEM fellowship program does not sponsor in-person visits or personally meet with current applicants outside of the official interview process. Applicants are invited to visit the city on their own, or if sponsored visits by the Department of Pediatrics become available, applicants will be notified by the program coordinator of these opportunities.
Fall Interview dates:
If you have questions regarding the application process, please contact our program coordinator, Jessica Coleman via email at jessica.coleman@childrenscolorado.org.
Do not send messages to the program through ERAS.
Salary and Benefits
The University of Colorado offers salary and benefits packages that are competitive with other fellowship programs across the country. Current salary levels can be found at the School of Medicine - Graduate Medical Education Stipends

Tien Vu, MD

Jason Woods, MD

Jessica Coleman
| Diversity / Equity / Inclusion |
We are committed to creating a diverse environment for students, residents, fellows, and faculty. We believe that an environment of inclusiveness and respect promotes excellence and that a setting where diversity is valued leads to the training of physicians who are prepared to practice culturally effective medicine and meet the needs of the various populations we serve. Visit our Diversity, Equity, and Inclusion webpage for more.... |
| Well-Being / Resilience |
By embracing wellness and improving personal resiliency, physicians can reconnect with the meaning of their work and fend off stress. Reducing or eliminating burnout also has practical implications for the entire department such as improving patient safety, student advancement, and the overall campus environment. Visit our Pediatric Well-Being and Resilience website for more. |
Pediatric Emergency Medicine Fellowship
Program Coordinator: Jessica.Coleman
13123 East 16th Avenue, Box
Aurora, CO 80045
Phone: 303-724-2566 | Fax:720-777-7258