Lab Overview
I am trained as a physiologist, with a focus on lifestyle interventions to reduce the risk of cardiovascular disease and kidney disease progression in patients with kidney diseases, particularly autosomal dominant polycystic kidney disease (ADPKD) and chronic kidney disease (CKD). Our laboratory conducts clinical and translational research in these populations, evaluating the efficacy of interventions, physiological mechanisms underlying pathophysiology, as well as physiological changes mediating improvements in response to interventions. Additionally, I completed a MPH in epidemiology, and I have a strong interest in translational research that spans from the cellular level to a population-wide impact.
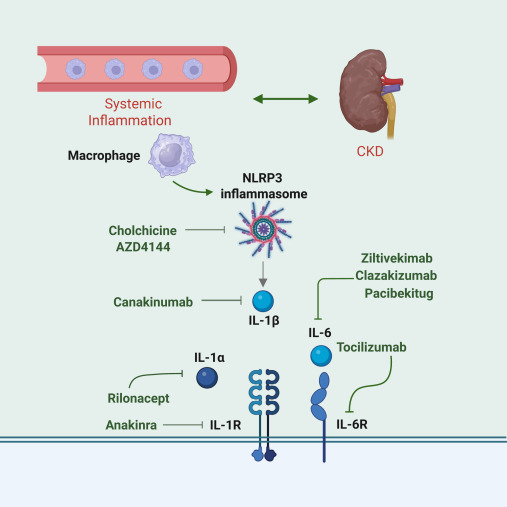
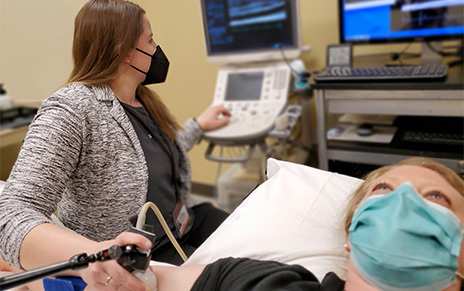
Our laboratory has equipment and expertise to employ state-of the art techniques, including measuring brachial artery flow-mediated dilation, carotid artery compliance, pulse-wave velocity, transcranial Doppler assessment of cerebrovascular reactivity, and functional near-infrared spectroscopy. Our integrative methods include oxidative stress-mediated suppression of endothelium-dependent dilation, vascular endothelial cell collections, serum incubation in cell culture, pro-inflammatory cytokine production of stimulated peripheral blood mononuclear cells, and adipose tissue biopsies.
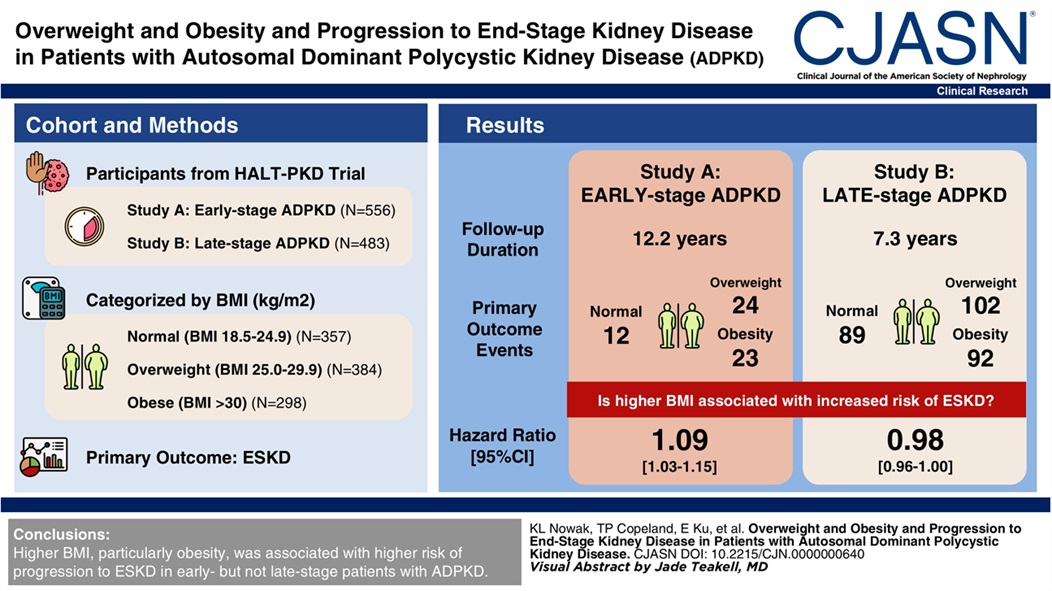
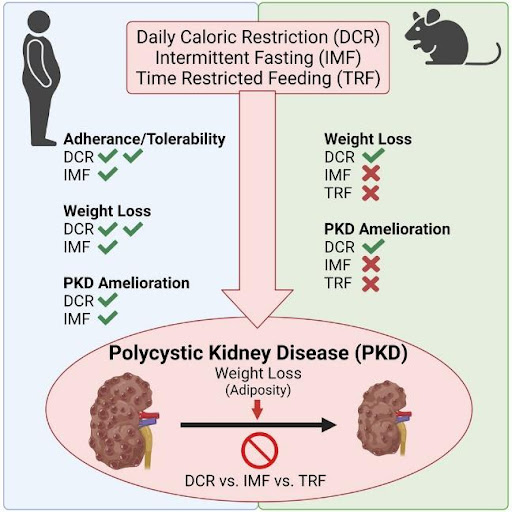
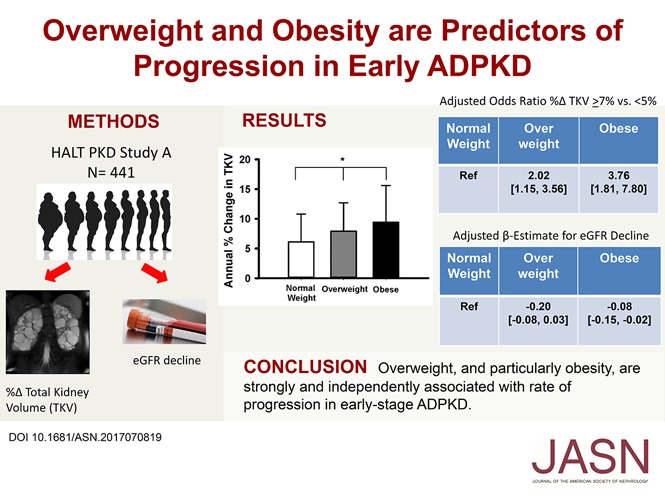
In addition to expertise in vascular physiology, we are actively investigating strategies targeting metabolic reprogramming (e.g., caloric restriction) and adiposity in adults with ADPKD. We are at the forefront of novel ADPKD research and clinical trials. For example, we were the first to report a strong and independent association between overweight and obesity in ADPKD progression, and our research in this area has been incorporated into the 2025 KDIGO Clinical Practice Guideline for the Evaluation, Management, and Treatment of ADPKD. I have been PI or Co-I for multiple clinical trials in patients with ADPKD, as well as CKD, including children and young adults.
We are committed to the scientific training of the next generation. Trainees in the laboratory have successfully obtained individual postdoctoral fellowships and career development awards supporting their cutting-edge research.