
CHA/PA Program Overview
The three-year, innovative curriculum of the University of Colorado PA program is designed to integrate clinical and basic sciences to prepare graduates with the knowledge, skills, and attitudes to practice medicine as part of the health care team. Graduates practice in all areas of medicine and serve patients of all ages.
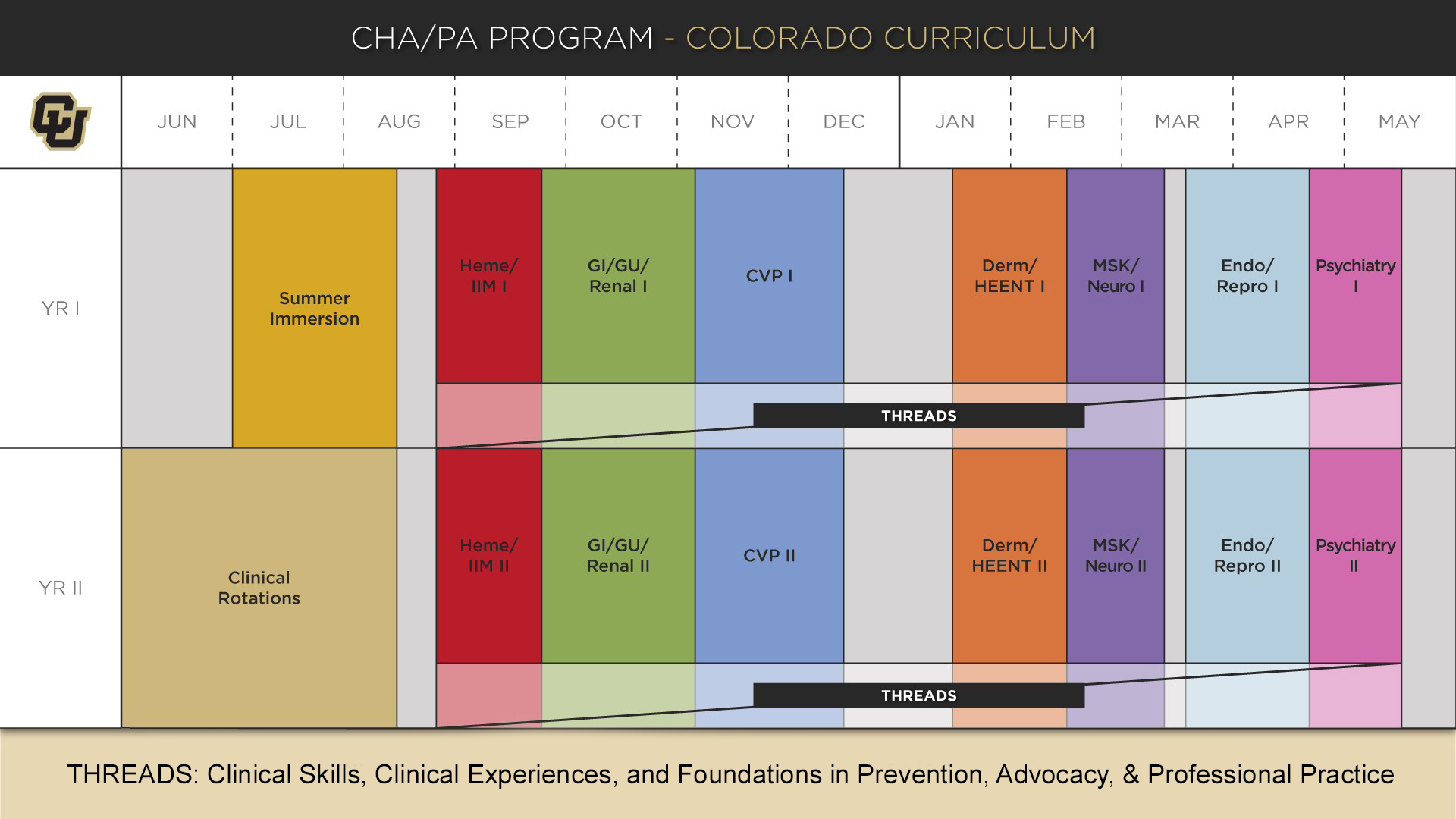
The information below pertains to the Colorado Curriculum, which was adopted in 2018 and applies to students graduating in 2021 and beyond.
The Colorado Curriculum is a cutting-edge, learner-centered educational platform designed to foster clinical decision-making and lifelong-learning skills. The curriculum is based on clinical presentations, which mimics how patients present for care and how clinicians practice medicine. For example, during the week of the curriculum focused on the clinical presentation “shortness of breath”, all learning in the basic sciences and clinical medicine is delivered in the context of a patient with shortness of breath.
The Colorado Curriculum consists of two didactic years, with clinical experiences integrated across both years. The third year of the program consists of 10 one-month rotations. The program begins in July with a summer immersion course that includes fundamentals of learning strategies, PA professional roles, wellness and resilience, and clinical topics.
The curriculum is organized into seven system-oriented blocks: Hematology, Infection, Inflammation and Malignancy (Heme/IIM); Gastrointestinal, Genitourinary and Renal (GI/GU/Renal); Cardiovascular and Pulmonary (CVP); Dermatology and Head, Eyes, Ears, Nose and Throat (Derm/HEENT); Musculoskeletal and Neurology (MSK/Neuro); Endocrinology and Reproduction (Endo/Repro); and Psychiatry. The curriculum is an iterative, spiral approach to learning, such that clinical topics which are introduced in the first year are often revisited at a more advanced level in the second year. Each block course integrates basic sciences and clinical medicine by employing the use of small group experiences, case-based learning, standardized patients (SPs), patient simulations, lectures, and collaborative, hands-on sessions. Additionally, students participate in thread courses over both years which provide education in clinical skills, role development, advocacy, patient care for diverse patient populations, wellness and preventive medicine, and early clinical exposures. The thread courses include Clinical Skills, Clinical Experiences, and Foundations in Prevention, Advocacy, and Professional Practice. See the individual course descriptions for further details on course content. An overview of the vision and goals of the Colorado Curriculum are illustrated in this LICENSE document.
Interprofessional Education and Tracks
Educational content is enhanced through the applications of family-centered care, behavioral and psychosocial perspectives as well as social and community initiatives for health and wellness. The program has integrated content in public health, oral health, professionalism, and interprofessional education. Students with a personal area of interest may also have the opportunity to participate in specialized tracks to enhance learning in adult hospitalized patients, pediatric critical and acute care, or rural health.
Clinical Experience and Affiliates
The curriculum includes fully integrated clinical experiences in hospital and community settings. During clinical experiences, students may observe a practitioner's practice, but may also participate in history-taking, physical examination and assessment,
development of a differential diagnosis and clinical decision-making and planning of treatments and interventions. Students work closely with preceptors and other members of the health care team and are evaluated on skills and competencies required
for patient care.
All rotations are scheduled by the Clinical Team based on accreditation standards, program requirements, track requirements, and preceptor/site availability. The Clinical Team is not able to accommodate specific requests for rotations, students will be scheduled in rotations in a variety of settings across multiple disciplines throughout their time in the program.
As a part of the University of Colorado School of Medicine, the faculty of the entire school of medicine and affiliates contribute greatly to the quality of the learning experiences provided at the CHA/PA Program. Affiliations with the University of Colorado Hospital, Children’s Hospital Colorado, and Denver Health and Hospitals in addition to community clinics, provide a network of clinical experiences to enhance the training of students. The faculty within the departments of Pediatrics, Family Medicine, Internal Medicine, Surgery, and others regularly participate in both classroom and clinical training of the CHA/PA Program students.
Degree
The University of Colorado PA Program has gained national recognition for its curriculum in primary care medicine. The Program confers a Professional Master’s Degree (MPAS). In accordance with the mission of the program, the CHA/PA Program curriculum provides comprehensive physician assistant education in primary medical care with additional training in pediatrics and disadvantaged, at-risk and medically underserved populations. There are specific requirements that all students must complete to receive the MPAS degree from our fully accredited PA Program. Graduates are well prepared to perform in primary care practice with patients across the lifespan. Historically our students have performed above the national average in score and passing rate on the National Commission on Certification of Physician Assistants (NCCPA) examinations.
Graduation and awarding of the Masters of Physician Assistant Studies is based upon the following requirements:
- Successful completion of all coursework and rotations of the University of Colorado PA Program
- Exhibiting professionalism throughout the course of study
- Successful completion of the Comprehensive Clinical Knowledge and Clinical Skills Examinations
In the first year of the program, student learning utilizes a variety of approaches including small group experiences, lectures, interprofessional sessions, laboratories and clinical experiences. Hands-on learning is gained through clinical skills and laboratory sessions in addition to direct clinical experience. Early clinical experiences begin in the 3rd semester to allow students to start practicing the skills they are learning in the classroom. Students must pass all first-year courses in order to be promoted to second year. Click here to see a list of the courses required for CHA/PA Students.
The third year (June through May) consists of ten, one-month long rotations and a one-month vacation that can be used to complete professional development modules, Capstone requirements, and self-care activities. The required rotations and elective rotations are dependent on the student’s track. All students, regardless of track, must complete one-month in either an out of metro area or medically underserved site.
Students complete a capstone project during year three, returning to campus during the final month of the program to present their topic as part of the Clinical Connections courses. The project represents a culmination of student progress through the program and allows students to identify a clinical case that illustrates a practice-based and/or systems-based approach to care.
Students are required to pass all 3rd Year clinical rotations, the requirements for Clinical Connections, as well as the 3rd Year comprehensive written (knowledge-based) and clinical (practice-based) exams consisting of knowledge and practical standardized patient exams in order to be eligible for graduation from the program.
Traditional Track — 35 Hours (Courses Are Subject to Change)
| Months | Type of Rotation |
| 1 month | Primary Care I |
| 1 month | Pediatric Specialty (e.g., Neonatology or Adolescent Medicine) |
| 1 month | Inpatient Medicine |
| 1 month | Primary Care II |
| 1 month | Emergency Medicine |
| 1 month | Primary Care III |
| 1 month | Surgery |
| 1 month | Primary Care IV |
| 2 months | Electives |
| 1 month | Vacation |
| Fall Semester | Clinical Connections I |
| Spring Semester | Clinical Connections II (with Capstone) |
Pediatric Critical & Acute Care (Courses Are Subject to Change)
| Months | Type of Rotation |
| 1 month | Primary Care I |
| 1 month | Pediatric Specialty (e.g., Neonatology and Adolescent) |
| 1 month | Inpatient Pediatric Medicine |
| 1 month | Primary Care II |
| 1 month | Surgery |
| 1 month | Emergency Medicine |
| 1 month | Primary Care III |
| 1 month | Primary Care IV |
| 1 month | Pediatric Critical and Acute Care Rotation |
| 1 month | Electives |
| 1 Month | Vacation |
| ** Students must complete Emergency Medicine and Inpatient Pediatric Medicine rotations prior to the Pediatric Critical and Acute Care Rotation. | |
Care of the Hospitalized Adult in a Novel Graduated Experience (Courses Are Subject to Change)
| Months | Type of Rotation |
| 1 month | Primary Care I |
| 1 month | Pediatric Specialty (e.g., Neonatology and Adolescent) |
| 1 month | Inpatient Adult Medicine-CHANGE Track |
| 1 month | Primary Care II |
| 1 month | Surgery |
| 1 month | Emergency Medicine |
| 1 month | Primary Care III |
| 1 month | Primary Care IV |
| 2 months | Electives |
| 1 month | Vacation |
Total credits vary based on track requirements.
* Subject to Change
The CHA/PA Program offers students the opportunity to participate in tracks to help personalize and extend learning beyond our standard curriculum. These tracks include exciting opportunities for interdisciplinary education, integrating students with others in the School of Medicine and across the campus with similar interests. Applications for placement in the tracks listed below occurs during the summer of the 1st Year.
Pediatric Critical and Acute Care Longitudinal Experience (PCACLE)
This longitudinal experience was developed by CHA/PA faculty and Children's Hospital Colorado faculty to meet the needs of students wishing to focus in pediatric critical and acute care. Students participating in the curriculum receive specialized instruction
and clinical experiences with critical care physicians and physician assistants at Children's Hospital Colorado and Denver Health. Additionally, students complete a customized curriculum through targeted readings and lectures. Continuity over the three years of the program helps to ensure growth and progression of clinical skills, clinical reasoning,
and autonomy. This individualized educational experience prepares students for careers in pediatric emergency rooms, intensive care units, and other acute
pediatric care settings.
The Pediatric Critical and Acute Care Longitudinal Experience is limited to 4 students per class.
Care of the Hospitalized Adult in a Novel Graduated Experience (CHANGE)
This longitudinal experience was developed by University of Colorado Hospital Advanced Practice Providers, in concert with CHA/PA faculty, to meet the needs of students wishing to focus on care of inpatient adults. Students participating in the curriculum receive continuity instruction and clinical experiences with APPs at University of Colorado Hospital over the three years of the program. This continuity helps to ensure growth and progression of clinical skills, medical reasoning, and autonomy. Additionally, students complete a customized curriculum through targeted readings and lectures. This individualized educational experience prepares students for careers in general hospital medicine, intensive care units, and consult hospital services.
CHANGE is limited to 2 students per class at this time.
Rural Health Track
The CHA/PA Rural Health Track is designed specifically for students who have a passion for serving underserved communities in rural areas. With the increasing demand for healthcare professionals in these regions, our program aims to equip students with the necessary knowledge and skills to make a meaningful impact. Key features of our Rural Health Track include the following:
- Didactic experiences designed to bring a rural focus to students’ healthcare studies
- Hands-on clinical experiences in rural clinics, hospitals and/or community health centers, when these sites are available
- Rural community engagement encouraging students to contribute to the improvement of community health
- Interdisciplinary training to ensure our graduates are prepared to address the challenges of rural healthcare
- Scholarship opportunities to ease the financial burden for students in exchange for a 2-year commitment to work in a rural healthcare setting after graduation
Guatemala International Experience
The CHAPA program provides an opportunity for students to complete a clinical rotation at the Trifinio Clinic in rural southwest Guatemala (a CU international site). Students in their second year may engage in a 4-week experience that begins with two weeks in a Spanish-language immersion program at Celas Maya followed by two weeks working in the rural clinic, caring for patients. This elective rotation focuses on pediatrics, women’s health, and family medicine. Clinical coursework involves observation and hands-on skills acquisition under the guidance of the medical team. Encounters may include home visits in conjunction with community nurses, specialty and/or hospital-based care. Students will have exposure to patients across the life span, provide care related to preventative, acute, chronic and/or emergent health conditions as well as provide education to patients on a variety of topics, including sexual and mental health.Fluent Spanish speaking students have an opportunity to return to the Trifinio Clinic for a one-month elective rotation in their third year.
Accreditation
The Accreditation Review Commission on Education for the Physician Assistant (ARC-PA) has granted Accreditation-Continued status to the Physician Assistant Program sponsored by the University of Colorado. Accreditation-Continued is an accreditation status granted when a currently accredited program is in compliance with the ARC-PA Standards.
Accreditation remains in effect until the program closes or withdraws from the accreditation process or until accreditation is withdrawn for failure to comply with the Standards. The approximate date for the next validation review of the program by the ARC-PA will be in 2026. The review date is contingent upon continued compliance with the Accreditation Standards and ARC-PA policy.