Behavioral Health Resources
Effective, sustainable weight management involves learning and then intentionally implementing healthy lifestyle behaviors, as well as an awareness for how things may throw us off track and how we can get back on track. Success can take time, planning, persistence, patience, and commitment to making healthy choices daily.
Having support around shifting habits and patterns of behavior is integral to achieve desired weight outcomes. This is where a Behavioral Health Provider (BHP) can be an effective part of the weight management team.
Overview of the role of the BHP in weight management
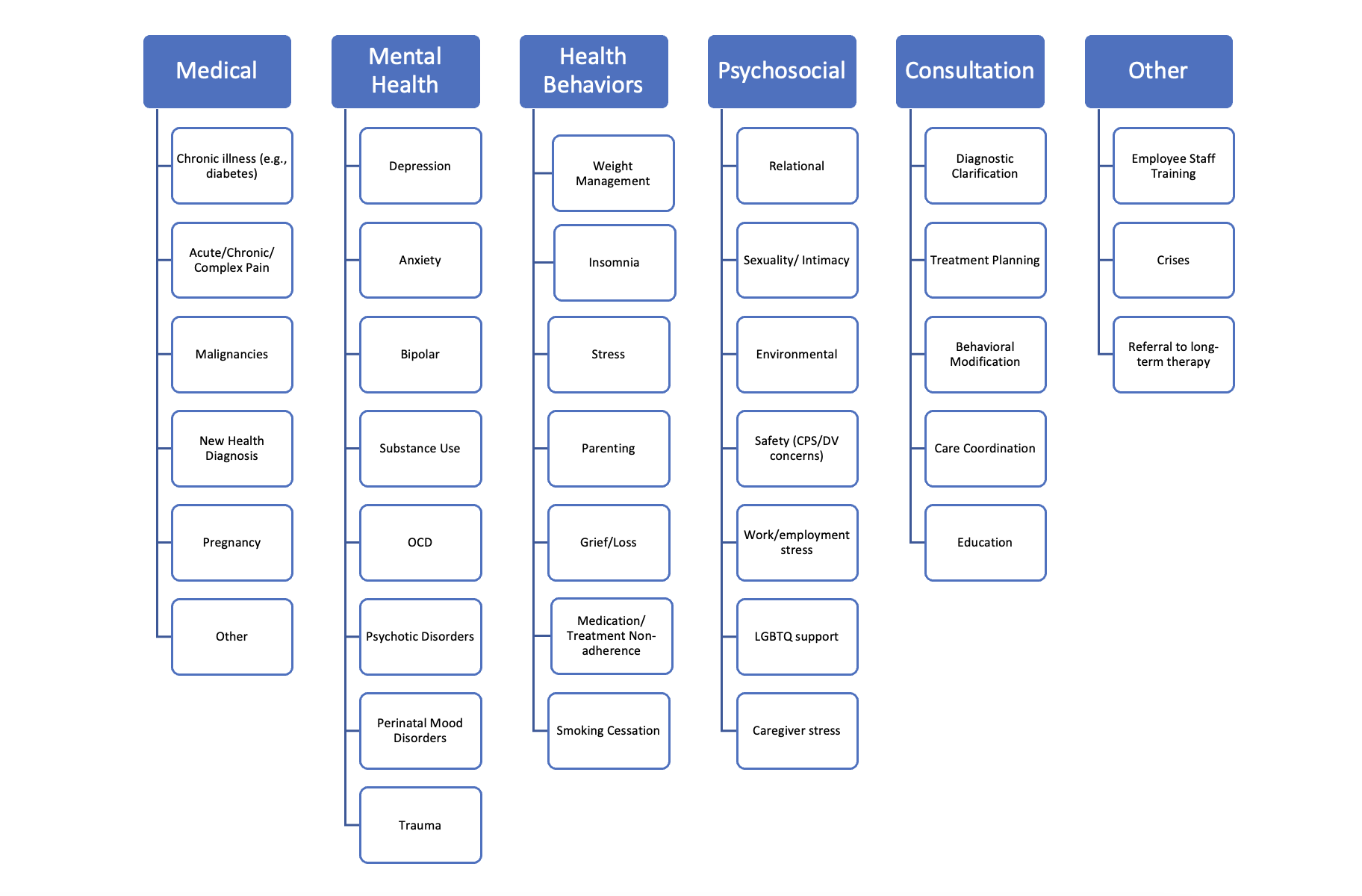
Not only are BHPs in primary care trained to support patients who may be struggling with a wide range of behavioral health concerns (e.g., depression, anxiety, trauma, substance use), but they can also help patients with health behavior change, including weight management. By targeting the behaviors associated with increased weight and collaboratively creating a plan with patients, BHPs can help patients transfer the what (what they need to do/eat/change) into the how. In some cases, patients need information on specifics (types of foods to eat/avoid) to be successful with weight loss. But many patients have a general understanding of what they need to be doing. Their challenge is putting this knowledge into practice and developing healthy habits.
Shifting into weight management for BHPs
For some clinics, using BHPs to help with weight management can be new. Here are some ideas to support your clinic in engaging BH support:
- Discuss with your clinic leadership team your interest in more weight management consults, and get their feedback on workflow considerations to support this.
- Present at a clinic team meeting how BHPs can be helpful in working with patients who want to focus on weight loss. Medical assistants can be helpful in pending BH referrals or alerting providers when patients indicate they might benefit from meeting with a BHP.
- Create handouts to remind providers about considering BHPs for their patients when they have a weight-prioritized visit.
- Scrub schedules and discuss with providers opportunities for warm handoffs.
- Make it patient-driven: include visuals or action plans that are readily accessible in exam rooms, like this one open. open new window
- Work with a physician champion to build up more consults with their panel of patients.
- Share success stories or tips on behavioral weight loss strategies through emails, newsletters, team meetings, etc. to keep the focus on this type of support.
Thinking about using your BHP to support weight management
Here are some tips to consider during weight-prioritized visits when you want to discuss using your BHP as a part of their care team:
- Language matters - it can be helpful to normalize seeing a BHP because, unfortunately, there can still be a stigma. Here are examples of scripting for this:
- “I have a colleague who specializes in behavioral strategies to support weight management that I would like to introduce to you today. Would that be ok?”
- "We take a team approach to weight management to fully support your health goals. One of my teammates focuses on strategies and behaviors to help you be most successful in achieving your goals. Would you like to meet her today?”
- Comorbidity problems can complicate weight management success. BH can help with these problems. Considerations include:
- Stress (job stress, family stress, relationship stress, life stress)
- Insomnia
- Emotional or stress eating
- Binge eating
- Sedentary lifestyle
- Substance use
- Depression
- Trauma
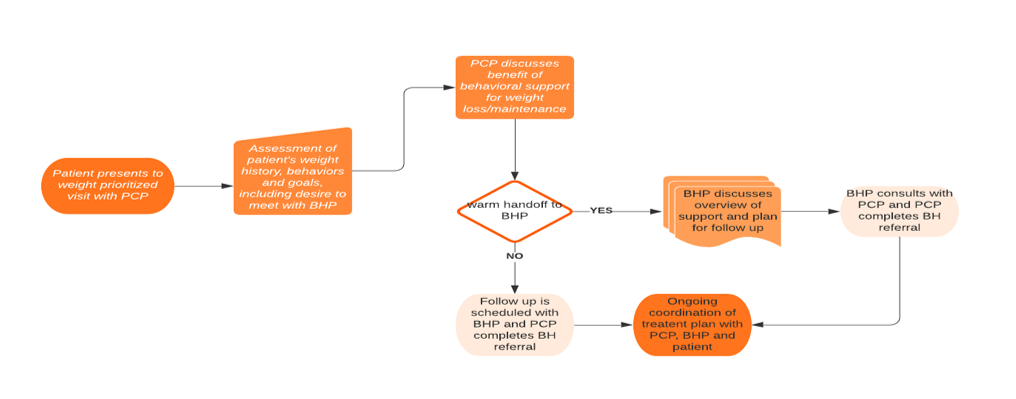
Example of a workflow to support team-based care with a BHP for patients prioritizing weight:
Considerations for an Initial Weight-Prioritized Behavioral Health Visit
Screening Tools
When having an initial weight prioritized visit, a BHP may choose to supplement screening tools they already use in primary care for common presenting concerns (i.e., GAD-7, PHQ-9, MDQ, PCL-5, AUDIT, DAST, etc.) with additional tools related to weight history and eating behaviors. This may include:
Eating Disorder Examination Questionnaire (EDE-Q)
Questionnaire on Eating and Weight Patterns -5 (QEWP-5)
International Physical Activity Questionnaire - Short Form
International Physical Activity Questionnaire - Short Form
Longer for more time: Weight and Lifestyle Inventory (WALI)
Quality of life or other measures related to the assessment of obesity and a discussion of their psychometric properties can be found here.
Evaluating Contextual Factors
In order to be effective in guiding individualized treatment, it is vital to have an understanding of the patients’ contexts for how their weight came to be a concern. This involves gathering a thorough biopsychosocial history with a focus on the patient's:
- Relationship to food (24-hour food intake recall)
- Weight history (When did this start? Has it been life-long or did it become harder as an adult or following critical periods - childbirth, surgeries, illnesses, etc.?)
- Family and cultural factors (family history of weight concerns, family behaviors around food, holiday meals, etc.)
- Current stressors
- Social supports
- Potential barriers
- Past successes or attempts at weight loss
- Current coping strategies (both healthy and potentially maladaptive)
Note that when the patient completes a weight-prioritized visit, many of these questions are in the PATHWEIGH questionnaire. The BHP may choose to review the patient’s answers and the clinician’s notes or may conduct additional assessments.
BHPs should use their typical scheduling and documentation templates for BHP weight-prioritized visits. WPV visit types are primarily used by PCPs
Behavioral strategies that are effective for weight management
A number of skills have been found to be effective when working with patients focusing on weight management. Here are just a few, with some additional resources provided. Note that these strategies are also included in the PATHWEIGH smart set for a clinician visit.
- Self-monitoring - tracking what are you eating, how much, when, and why can be a helpful foundation to assess what tweaks to start with. Monitoring itself helps us change what we do.
- Stimulus control strategies - setting our future selves up for success means creating an environment to help support us. This might be changing what’s available to eat (getting rid of the junk makes it harder to access) or other cues in the environment to help us be healthy (e.g., putting out our workout clothes the night before may make it more likely that we will get into them the next morning).
- Problem solving - planning and preparing for meals, fitting physical activity into a busy work week, and preparing for meals while at restaurants, on vacations, and during holidays all require problem-solving to stay on track.
- Cluing into hunger and satiety cues vs other reasons for eating - it’s not uncommon to use food as a coping strategy. Supporting non-food related coping skills can help individuals self-soothe that won't derail their lifestyle.
- Relapse prevention - patients can learn how to recognize when their behavior goes off track and how to readjust to continue maintaining behavior changes.
For additional tools and links to weight management handouts, download the behavioral health toolkit. open new window
Behavioral Health toolkit video
Behavioral health billing for weight management
To make engagement in behavioral weight management support for your clinic sustainable, ensure that billing practices support the work. Billing for BHPs in integrated primary care settings depends on a number of factors including state guidelines, credentials, and type of visit. Psychotherapy codes (90791; 90832; 90834; 90837, etc.) require a mental health diagnosis. Patients who have a comorbid mental health diagnosis that is impacting their ability to successfully manage their weight might qualify for this type of billing. Absent a mental health diagnosis, there may still be patient behaviors or psychosocial concerns that are impacting a medical condition. Psychological Factors Affecting a Medical Condition (PFAMC; F54) is one such diagnosis that may be pertinent in situations in which a patient’s behaviors are affecting weight.
Health and Behavior Codes are also available to bill for medical conditions as primary to the visit. Further information on billing for behavioral health can be found below:
Talk with your billing and coding specialist to investigate options for reimbursement available at your practice and to ensure that the appropriate authorizations are done when referring patients to your BHP.
Additional resources for Behavioral Health Providers
Training and Webinars
- Beck Institute: CBT for Weight Loss and Maintenance Training
- Society for Behavioral Medicine Trainings and Webinars
- Association for Behavioral and Cognitive Therapies Trainings and Webinars
Additional resources for Primary Care Providers
If your practice doesn’t have behavioral health but is interested in including a BHP as a part of your care team, there are many online resources and toolkits that have been developed to support practices in navigating this. Resources range from decisional support tools on the type of model that would work best for your practice to how to recruit a BHP in your community.
- Behavioral Health Integration Tools and Resources
- Quick Start Guide for BH Integration for Safety Net PCPs
Tips for Primary Care Providers on supporting patients with weight loss
It is important to build comfort in approaching and discussing strategies to manage weight with patients. Practice and get familiar with key phrases that bring this topic up in a non-judgmental, compassionate, and solution-focused way. Below are some suggestions to help you start this conversation, as well as tools to support using motivational interviewing strategies to discuss weight management with patients.
- Talking with Patients about Weight Loss: Tips for Primary Care Providers
- Tips and Resources to Help Patients Live a Healthy Lifestyle
- The 5As Framework and Motivational Interviewing Strategies for Discussing Weight Management with Patients
Community Behavioral Health Resources
- www.Psychologytoday.com - offers a directory of mental health providers that you can filter by location, insurance, type of therapy offered, etc.
- Colorado Department of Human Services – linkages to Colorado community mental health centers, the CO Crisis Service, and additional substance use providers.
- Please click here for a list of community resources located in the State of Colorado open new window