Welcome to Cheryl Ackert-Bicknell Lab
Lab Director, Cheryl L. Ackert-Bicknell, Ph.D.
Our Research
Genetic Regulation of Bone Research at University of Colorado's Ackert-Bicknell Lab
Osteoporosis is a complex disease of decreased bone mass resulting in fracture that is estimated to affect over 12 million Americans. Numerous studies have shown that osteoporosis is largely a genetic or familial disease. Our lab uses a number of strategies to identify the gene that are associated with osteoporosis and the environmental factors that interact with these genes to alter bone mass and strength. In addition, we study the diagnosis of and the consequences of postoperative infection, with an emphasis on an infection associated with spinal instrumentation.
Our main research areas are:
Topic Areas:
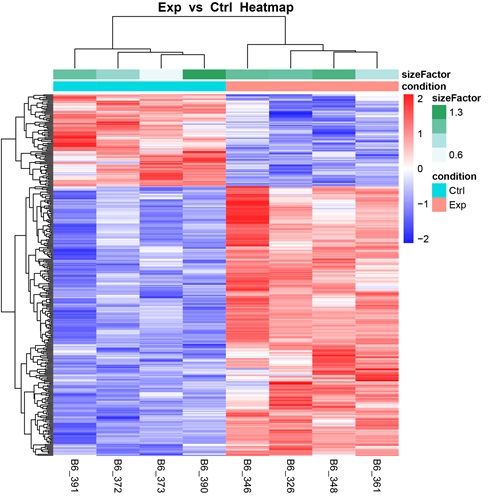
System Genetics
The goal of this project is to genetically dissect one of the most important processes affecting bone, osteoblast-mediated bone formation. We hypothesize that by focusing on a cellular phenotype and employing systems genetics methodologies, we will have increased success in discovering genes that specifically modulate bone formation, as compared to traditional mapping studies of higher-level phenotypes.
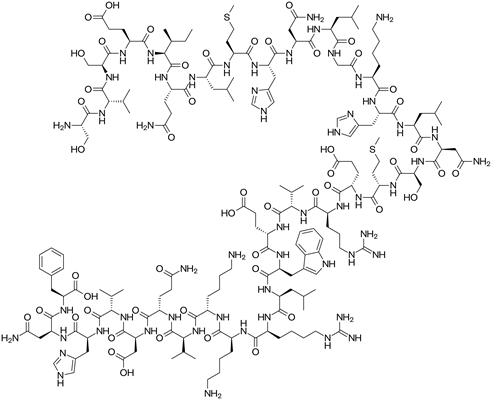
Gene by Environment Interactions in Bone
Our lab is interested in identifying genes that participate in the regulation of bone mechanical integrity and bone mass but do so via interactions with environmental modulators. We are specifically interested in determining how the in-bone actions of pharmacological factors such as Teriparatide, a PTH analog (pictured), are modified by genetic factors. In addition, we are also interested in the impact of dietary fat on osteoblast and osteocyte function in the face of allelic differences.
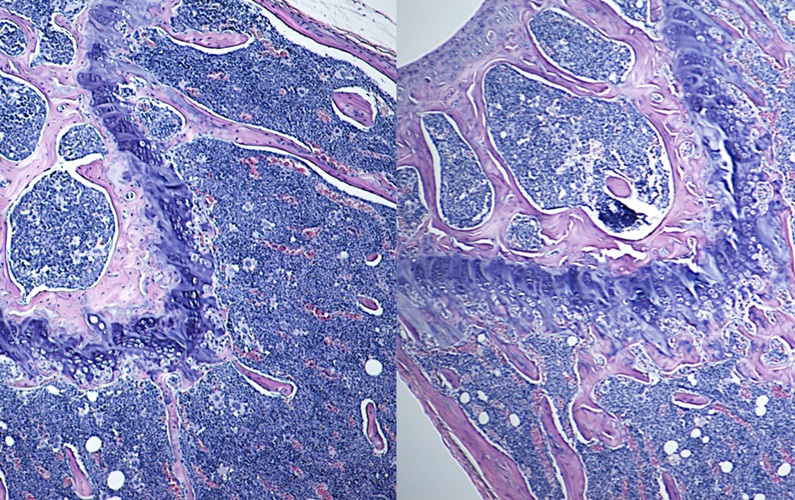
Functional Validation of GWAS Loci
To date, over 500 bone mineral density loci have been identified via Genome-Wide Association Studies (GWAS) in humans. As we enter the “post-GWAS era,” the focus is now shifting towards understanding how the underlying gene or genes act to modify bone. We use in vivo and in vitro models to determine the biological function of uncharacterized candidate genes for bone mineral density, bone formation, and bone strength.
Spine Infection Diagnosis
Surgical site infections of the spine associated with implanted orthopedic devices are difficult to diagnose and even more difficult to monitor during treatment. In this study, we seek to determine if we can leverage circulating antibody-producing cells obtainable from routine blood samples to diagnose and monitor surgical site infections of the spine caused by Staphylococcus aureus. The goal of this work is the creation of a simpler, less expensive, and faster diagnostic tool that can lead to earlier interventions and better outcomes for spinal infection patients.
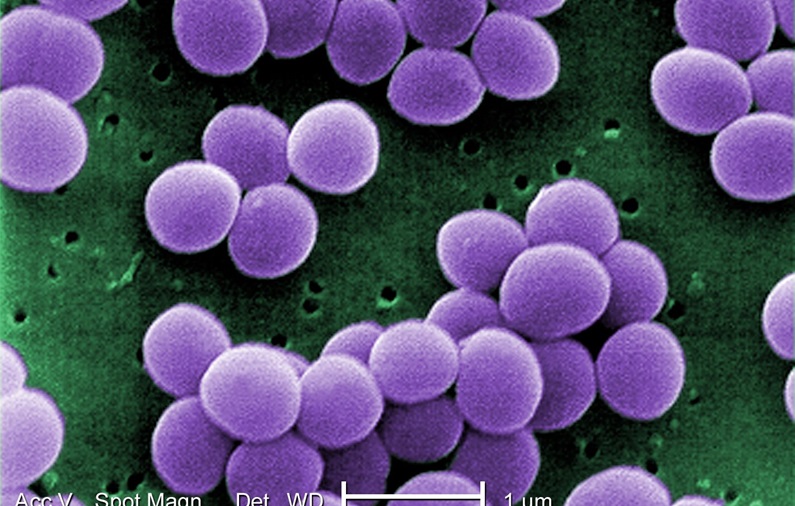
Bacterial Mediated Corrosion
Dr. Ayers is the project lead for this study. The presence of metal ions or particles in tissue coming from a metal implant has been termed “metallosis” and is considered by the FDA to be a significant health risk in patients. All orthopedic biomedical alloys, oil pipelines, chemical plant pipes, and industrial heat exchangers suffer from corrosive degradation over time and this is often associated with the presence of microbial populations. The goal of this research is to test for bacterial involvement in spine implant corrosion and explore the biofilm associated with metallosis.