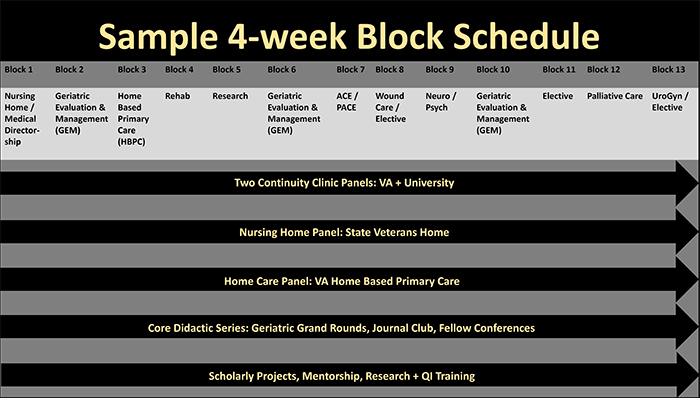
Geriatric Evaluation and Management (GEM): 3 blocks per year. The GEM months focus on the care of geriatric patients in the post-acute care setting, with emphasis on optimizing transitions from hospital to facility and from facility
to home. This rotation also serves as a primary teaching service for Internal Medicine residents, Med-Peds residents, and Primary Care interns, offering fellows the opportunity to serve as team leaders, supervise clinical care, and provide education
to trainees.
Home Based Primary Care (HBPC): 4 weeks per year and longitudinal. Early in the year, fellows will experience the collaborative, interdisciplinary approach of the VA HBPC team and acquire 2-3 continuity patients to follow throughout
the fellowship. During the month-long rotation time is spent with an attending physician doing admissions and establishing skills to see patients independently in the home, as well as experiencing visits with other team members including occupational
therapy, social work, and nutrition and participating in the weekly HBPC interdisciplinary meeting. Fellows then continue to follow continuity patients once every month throughout the year and attend HBPC meetings once every 1-2 months to present
the plan of care for their patients. Both the HBPC month long rotation and continuity experiences are anchored by didactic and group educational activities focused on core home care topics including home safety and adaptive equipment, home health
care and community resources for homebound patients, transitions of care, nutritional assessment and food security, and social determinants of health.
Palliative Care: 4 weeks per year. Fellows complete 2 weeks of inpatient consults and 2 weeks of outpatient palliative care clinic. During this rotation, fellows gain knowledge and skills to expertly manage patients with serious
illness through a team based approach with collaboration from social work, psychology, nursing, and chaplain providers. Skills gained from this rotation include navigating family meetings, goals of care conversations, advance care planning, and determining
hospice eligibility. In addition to assessing and treating both chronic and acute pain, training includes the art of providing relief by gaining knowledge on the psychosocial and spiritual aspects of suffering.
Community Nursing Home/Medical Directorship: 4 weeks per year. Fellows learn the administrative and leadership responsibilities involved in the Medical Director role while working with community-based providers in a variety of community
nursing home settings. This rotation offers fellows exposure to a variety of clinical and career models to demonstrate the potential for incorporating Medical Directorship into their future careers. Through participation in administrative meetings,
fellows learn approaches to quality assurance and patient safety in the long-term care setting.
Rehabilitation: 4 weeks per year. Fellows will learn alongside our Physical Medicine and Rehabilitation specialists the geriatric approach to peripheral joint injections, trigger point injections, musculoskeletal ultrasound, EMG
for neuropathy evaluations, spasticity management and interventional spinal therapeutics. During this rotation, fellows also work with physical and occupational therapy in both inpatient and outpatient settings to gain insight into the roles of these
important interprofessional collaborators.
Neuropsychiatric Medicine: 4 weeks per year. Fellows will spend time in a variety of settings with neurology, psychiatry, and psychology providers to learn about the geriatric approach to cognitive and movement disorders. Fellows
gain exposure to management of late-stage movement disorders through work in VA and University Neuropalliative Care Clinics. Fellows have the opportunity to work with a Behavioral Neurologist specializing in frontotemporal dementias and primary progressive
aphasias, who is involved in clinical trials with the University of Colorado Alzheimer’s and Cognition Center. Fellows will also spend time with a VA geropsychologist performing neuropsychiatric evaluations and providing support and counseling
to patients and caregivers. Additionally, fellows will spend time with a VA geropsychiatrist performing dementia and psychiatric evaluations of older adults at the VA site and in the community nursing home setting. During the rotation fellows also
have exposure to VA Dementia caregiver support groups and capacity evaluations.
Program for All-Inclusive Care of the Elder (PACE): 2 weeks per year. The CU Geriatric Medicine Fellowship partners with two Denver Metro area PACE programs: Tru Community Care and InnovAge. Fellows will spend 2 weeks working in
an interprofessional team environment at PACE. During this rotation, fellows participate in care across a spectrum of locations including PACE centers, nursing homes, locked memory unit, and assisted living facilities. This comprehensive care model
for dual eligible (Medicare and Medicaid) patients provides a unique opportunity for fellows to experience a community based multidisciplinary approach to geriatric care.
Acute Care of the Elder (ACE): 2 weeks per year. The ACE inpatient service is a primary teaching service for residents and students at University Hospital providing care to hospitalized older adults. Fellows participate in interdisciplinary
team meetings and rounds each day and provide geriatric teaching to residents and students during this rotation, serving as a geriatric content expert for the team.
Wound Care: 2 weeks per year. Fellows will learn to diagnose, investigate, and treat different types of wounds from specialists at the VA in both the inpatient and outpatient setting. Fellows learn when and how debridement is appropriate
and apply knowledge to wound healing for the selection of dressing and other topical wound care products and devices. Fellows leave this rotation trained to apply evidence-based medicine to complex wound care.
Urogynecology: 2 weeks per year. Fellows will spend two weeks in urogynecology clinics learning a multidisciplinary approach to care including collaborative care with colorectal surgery specialists. Fellows learn basics of pessary
fitting and management and core concepts related to the care of older adults with incontinence.
Elective: 6-8 weeks per year. Fellows can tailor their elective experiences towards a particular area of clinical interest, to fill gaps in knowledge, or for career planning and exploration.
Research: Each fellow receives protected time to complete Quality Improvement and other scholarly projects, either in a block rotation or a longitudinal model, depending on the fellow’s needs and interests.