Shared Content Block:
Styles -- custom quote
Shared Content Block:
Styles -- "spaced-out" class
Shared Content Block:
Styles -- "smart float" for images
Shared Content Block:
Styles -- restore normal formatting to bulleted and numbered lists
Model: Integrated — Incorporated in with Other Patient Care

In this model, you “blend in” weight management visits with patients during your regular patient care time. As the clinician, you see patients for a variety of different issues, including weight management, throughout your day.
Why you might want to choose this model:
- Patient visits for obesity can be blended in with other patient care and not require a separate carve-out program, additional time, or extra staff to do this.
- You don’t have many obese patients that you plan to treat in your practice and don’t plan to see patients outside of your primary care panel.
- You don’t want to set up a different system or workflow.
- Your medical providers are interested in directly addressing weight management during patient visits.
What you have to have to make this work:
- A knowledgeable care provider to see patients individually.
- Time available/capacity to regularly see obese patients for counseling; if you are already having trouble having open slots for patients to see your medical providers, this can be challenging as weight management involves regular visits over time.
How to pay for it:
- Coverage for obesity and weight management services is complex, and provider payments depend on each patient’s health insurance plan
- Medicare and Medicare Advantage plans cover IBT for obesity either in one-on-one 15-minute sessions (G0447) or 30-minute group sessions with 2 to 10 patients (G0473)
- In 2020, on average, Medicare paid a non-facility fee of $27 for G0447 and $13 for G0473
- Private plans may also cover obesity and weight management services under preventative medicine codes (99401-99412), group counseling codes (99078), Medical Nutrition Therapy codes (97802, 97803, 97804, G0270, G0271), or weight management/nutrition services provided by a non-physician (S9452, S9470, S9449, S9452)
- Many obese patients have other conditions that qualify for services that can be billed to a patient’s insurance plan under other procedure codes
- Medicare beneficiaries with a diabetes or renal disease diagnosis or a kidney transplant in the last 3 years are eligible for Medical Nutrition Therapy (97802, 97803, 97804, G0270, G0271)
- Patients can always self-pay and may have co-insurance or co-pays even if their insurance plan covers the service
Who can do it:
- Providers that can bill for obesity and weight management services depend on both the service and the patient’s health insurance plan
- Medicare permits primary care providers (physicians, NPs or PAs) and other providers as incident to a primary care provider to bill for delivering IBT for obesity
- Dietitians are allowed to bill for Medical Nutrition Therapy
- Other payers usually have credentialing requirements for professionals to bill for obesity and weight management services
What this model looks like in action
Patient story
This story is based on actual patient-care experiences but is fictional. Any resemblance to real persons is purely coincidental.
Dr. Adams is the sole clinician of a small family medicine practice. She firmly believes that obesity management is critical for her patients' long-term health and should be addressed in the primary care setting.
She is completing a Well-Woman Visit with Dana, who has chronic pain related to obesity. Dana is open to a conversation about weight management, as she feels her quality of life has suffered, and she's not able to take care of herself in the manner that she'd like.
To create a comprehensive plan of action, Dr. Adams orders blood work to be completed before Dana's next appointment, including a metabolic profile, lipid profile, and thyroid function tests.
During the visit, Dr. Adams completes an exhaustive medical history, including diet, nutrition, and physical activity assessments. She looks for signs or symptoms indicating Dana might have undiagnosed causes or comorbidities related to obesity (i.e. obstructive sleep apnea, polycystic ovary syndrome). Dr. Adams also reviews Dana’s medication list to see if any of her medications could be contributing to her weight struggles and whether there might be other alternatives. She also queries Dana's perceived barriers and facilitators to change and tries to understand how confident Dana is about making such changes. The two create short- and long-term goals to guide their efforts, using the SMART goal framework (https://www.rethinkobesity.com/talking-with-patients/setting-smart-weight-loss-goals.html). All of Dana’s results come back without the need for additional work-up.
Dana commits to frequent follow up appointments with Dr. Adams to assess her progress and make changes to her action plan as needed. Dr. Adams' assistant reaches out to Dana between appointments to provide support as needed. Since Dana also has hypertension and along with chronic pain, Dr. Adams can treat these comorbidities and bill Dana's insurance for chronic disease visits while she provides support and guidance about weight.
Dana sticks to her diet and exercise regimen by tracking using a free app downloaded on her smartphone. Dana and Dr. Adams begin with meeting every other week and then space out to once a month. By three months, Dana is starting to notice improvements in her health problems just by losing 7% of her body weight.
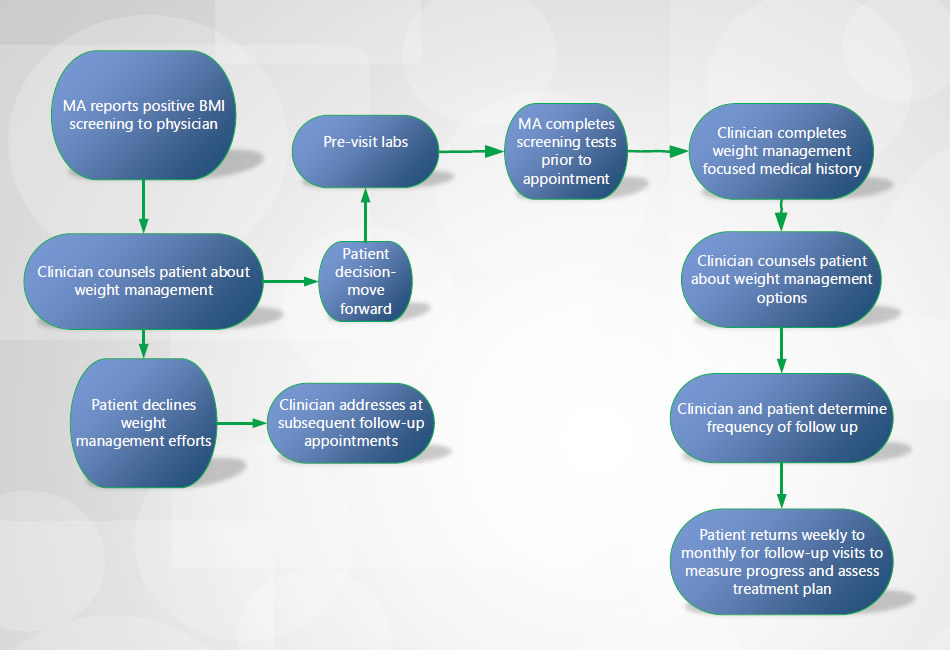
Flow diagram
Based on our research, we created this diagram of a typical workflow. This is simply an example of a starting point to consider. You should create a workflow that accommodates the functioning of your practice.
FAQ
I feel like one of my roles is identifying that there’s a problem and having that open, honest conversation with patients and trying to get their buy-in to getting help achieving a healthy body weight. And then also, you know, routine follow-ups, so that we can track their progress, provide encouragement, and refer them to people that can help them.
Physician
I think it helps from a standpoint of they’re being listened to, and it’s not just a ‘count your calories and you’re done’ type thing. I think if you can spend the time with the patients and help them brainstorm with their own personal roadblocks, then they see that you’re invested in their success, and they’re more likely to go home and actually implement the things that you discussed.
Physician
When the patient comes in, we evaluate... what needs to happen first. What’s most important for this patient? Sometimes weight management is discussed on the first visit if there are no active medical things going on, but if there are active medical things going on, we deal with those first and then say, hey, why don’t we schedule an appointment to talk about weight management?
Physician