Shared Content Block:
Styles -- "spaced-out" class
Shared Content Block:
Styles -- custom quote
Shared Content Block:
Styles -- "smart float" for images
Shared Content Block:
Styles -- restore normal formatting to bulleted and numbered lists
Model: Hire a Registered Dietitian Nutritionist (RDN) or Other Professional

In this model, instead of the weight management being primarily provided by the clinician (physician or advanced practice provider), it is provided by another role trained in weight management. We have seen these other professionals include (most often) an RDN (certified nutrition professional) and others such as a health educator, food scientist, or behavioral health provider (like a clinical social worker or psychologist).
Why you might want to use this model:
- If no one in your practice has the expertise to deliver weight management services, then hiring someone who does might be ideal
- RDNs have special training regarding nutrition and are likely to deliver evidence-based advice. However, seek an RDN who also has behavior change training to address the motivational and organizational issues with changes needed for weight management.
- Behavioral health providers are specially trained in behavior change, especially those with special training in health psychology; however, others may be needed for assistance with specific diet plans.
- Because these types of professionals may not be available in your area, some practices have benefitted from having food scientists, health educators, or health coaches fulfill this role. However, billing options may be limited.
- Adds the capacity to see more patients if your practice is very busy.
What you have to have to make this work:
- If you choose the RDN route, you need an RDN who has the knowledge and skill to do this. Most RDNs are wonderfully prepared to provide weight-management assistance to patients. They have excellent nutrition knowledge as well as the ability to fully engage with, listen to, and provide behavior change support for patients. However, not all are ideal for this role. Some do not have enough training in weight management methods to be successful. Some have a “tell people what to do” approach that doesn’t support individual patient behavior change. Some may not have enough training in behavior change to help patients progress with the behavioral aspect of weight management treatment. In our research, we have found that many RDNs have weight issues themselves, affecting the patient perception of credibility when counseling about weight management.
- If you choose a behavioral health professional (BHP), you need a recommended weight management program that patients can follow. The BHP then works with patients more on the behavior change aspects (e.g., helping patients set behavioral-change targets or goals and learn self-management techniques for weight management). The BHP often meets with a patient for 2-3 sessions or more lasting 20-30 minutes each.
- Space for the RDN or other professionals to work with patients OR a virtual visit set up to conduct visits via telehealth.
- Willingness to identify and refer patients while “endorsing” this person. They will need this steady stream of people coming from the medical providers to have patients to counsel, which may include other types of services beyond weight management, such as other nutritional or behavioral health support.
- The “other professional” should be advanced and independent enough to set up the program and make it work with the practice leaders’ and clinicians’ support, or you’ll need someone to coordinate these efforts.
How to pay for it:
- RDNs can bill Medicare and Medicare Advantage plans for delivering IBT as “incident-to” a primary care provider at the same rates of $27, on average, for G0447. However, providers using this model reported that the visit usually takes longer than 15 minutes, and the physician needs to be present.
- RDNs can bill directly for medical nutrition therapy, usually for a total of 3 hours in the first year and 2 hours in subsequent years. Medicare only pays for medical nutrition therapy if there is another condition, such as diabetes and chronic kidney disease. On average, Medicare pays $38 for the initial 15-minute visit (97802), $33 for each subsequent 15-minute visit, or $17 per beneficiary for 30-minute group sessions.
- Some private plans permit credentialed licensed clinical behavioral health providers to bill for weight management or nutrition services provided by a non-physician (S9452, S9470, S9449, S9452). The BHP can bill the following Health Behavior CPT Codes: 96156 (Health behavior assessment or re-assessment), 96158 (Health behavioral intervention, individual, F2F, initial 30 minutes) and 96165 (for each additional 15 minutes), listing separately in addition to code for primary CPT code. See https://www.apaservices.org/practice/reimbursement/health-codes/descriptors.pdf for more information.
- In addition, some private payers may permit "incident-to" billing for preventative medicine codes (99401-99404, 99411-99412).
- Some private plans may require a patient co-pay or co-insurance payment in these situations.
- Patients can self-pay. This usually doesn’t work, especially in areas with lower-income patients, as patients are not able to or do not perceive the value of having RDN counseling as something they should pay for.
Who can do it:
- RDNs and/or BHPs or other trained professionals depending on the scope and nature of the training.
- RDNs have the requisite training on nutrition management as per their license.
- The BHP should be a licensed clinical social worker or licensed clinical psychologist (so that they can bill Medicare and other insurance). Ideally you want a BHP with prior experience working in integrated primary care settings in a PCMH model and who has the following integrated care competencies: 1) identifying, triaging and co-managing patients with medical and behavioral health problems within the primary care setting; 2) providing skill training through psycho-education and patient education strategies and developing specific behavioral change plans for patients and behavioral health protocols for target populations; 3) assisting primary health care providers in recognizing and treating mental disorders and psychosocial problems, and behavioral medicine problems.
What this model looks like in action
Patient story
This story is based on actual patient-care experiences, but is fictional. Any resemblance to real persons is purely coincidental.
Marcus, a patient of Dr. Palmer since 2015, has come in for his annual wellness check. He has steadily gained weight over the years and recently developed pre-diabetes. Dr. Palmer presents his findings and concerns, making sure to do so in a non-judgmental manner. He asks Marcus about his interest in addressing his weight. Marcus says he'd like to try, so they schedule a follow-up appointment to discuss options.
Dr. Palmer's practice uses the "Other Professional" model in which a registered dietitian nutritionist (RDN) is employed by the practice to help patients with weight management. The practice also has a behavioral health provider (BHP) who can provide behavioral support change. At the follow-up visit, Dr. Palmer and Marcus develop a personal goal and create an action plan by considering available options and resources. Marcus chooses to schedule consults with the RDN and BHP and ultimately sees each professional on a bi-monthly basis.
At three months, Marcus returns to see Dr. Palmer to evaluate his progress. The RDN and BHP notes indicate that Marcus is making nice progress on his goals, sentiments that Marcus echoes during the appointment. However, he's having some difficulty with a weight plateau, so Dr. Palmer adds a short-term weight loss medication to his treatment plan and recommends strength-training. They have a follow-up visit a month later regarding his progress, and Marcus has started losing weight again.
At six months, Marcus has made enough progress to feel comfortable working with Dr. Palmer alone, knowing that he has professional resources if needed.
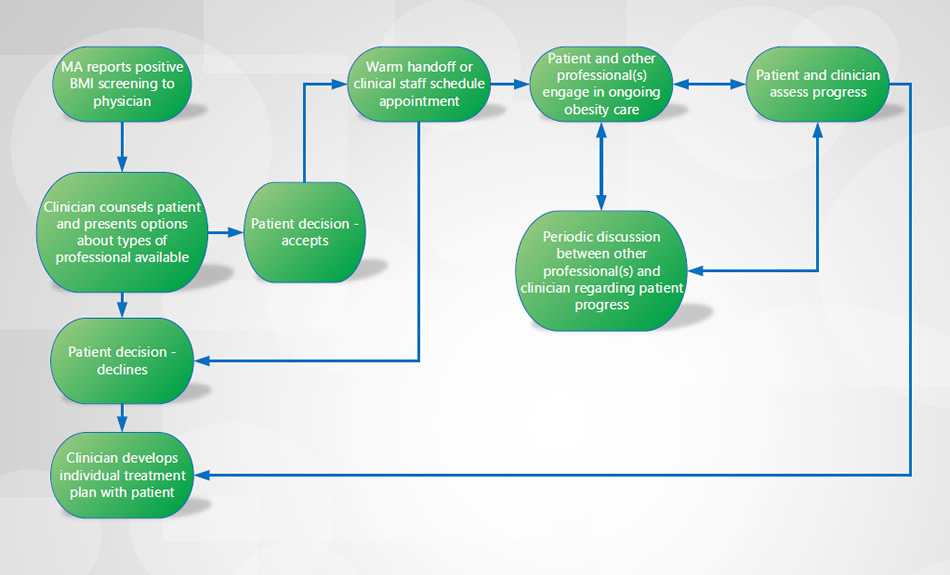
Flow diagram
Based on our research, we created this diagram of a typical workflow. This is simply an example of a starting point to consider. You should create a work flow that accommodates the functioning of your practice.
FAQ
The clinician’s piece of [weight management] could be fairly brief once things get rolling, so the therapist or the counselor or the life coach is going to conduct the bulk of the visit, but patients like to know that we’re involved. They like to be able to ask us a question, and if we are working to decrease medications, they want to be able to follow up on that. It’s variable, but the clinician's involvement decreases over time because the bulk of the work is being handled by the counselor.
Physician
The first thing I think of is our dietitian... I think [she’s] a great resource, and I’m so excited to be working with her. In residency, at the hospital, we had dietitians, but it was like a hassle to refer people. It just wasn’t used. So, having the dietitian right here, having her talk to people at their Medicare Wellness or their annual physical, is beneficial as a starting point to get everybody thinking about their diet. But then people that are overweight or obese, I can send them right over to her, which is super helpful.
Physician