Lab Overview
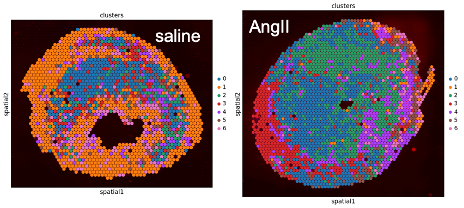
Mary C.M. Weiser-Evans is the Charles Boettcher II Professor of Medicine in the Division of Renal Medicine and Hypertension at the University of Colorado Anschutz Medical Campus. For more than 25 years, the research in the Weiser-Evans laboratory has focused on vascular biology, with particular emphasis on smooth muscle cell (SMC) signaling and understanding the regulation of SMC phenotypic modulation in disease. The laboratory has developed novel genetic mouse models that allow inducible smooth muscle-specific knockout or overexpression of specific genes involved in progression of vascular disease. We routinely use a SMC fate-mapping approach developed in our lab to track mature SMCs in the setting of disease progression even if SMCs lose all detectable expression of traditional SMC markers. This approach facilitates molecular analyses such as scRNA-Seq, ChIP/ChIP-Seq, and CyTOF mass cytometry. In vivo mouse genetic approaches are complemented by in vitro studies using cultured SMCs as well as co-culture systems that allow us to examine crosstalk between SMCs and inflammatory cells (e.g. macrophages).
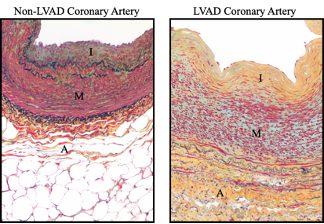
The lab has been particularly interested in the role of the tumor suppressor PTEN as essential for directing SMC differentiation. We were one of the first to identify PTEN in SMCs as an essential regulator of pathological vascular remodeling and our most recent studies defined a novel function for PTEN in the nucleus as an essential transcriptional co-factor with SRF in the regulation of the SMC differentiation program. Importantly and clinically relevant, studying normal and diseased human coronary arteries, we established that loss of PTEN expression directly correlated with SMC dedifferentiation and atherosclerosis progression and complexity. An additional area of focus and serendipitous findings using fate-mapping approaches demonstrated that mature SMCs are genetically reprogrammed to give rise to a select subpopulation of resident adventitial vascular progenitor cells (AdvSca1-SM cells). We showed that adventitial SMC-derived stem cells are the predominant cell type responding to vessel wall dysfunction and matrix production. Ongoing studies are focused on defining the mechanisms driving SMC reprogramming, determining the distinct functions of adventitial SMC-derived stem cells in the maintenance and repair of the vessel wall as well as their role in disease progression, and determining their therapeutic potential in vascular repair, bioengineering of blood vessels, and in the revascularization of ischemic tissues. In addition to vascular biology-related studies, collaborative studies have been focused on defining the role of the tumor microenvironment in lung cancer progression and metastasis. We developed a novel lung cancer metastasis model that allows us to examine the role of the lung tumor microenvironment on lung cancer progression, to define specific signaling pathways activated in both cancer cells and the tumor microenvironment that regulate cancer progression, and to test potential therapeutic agents. Using our novel AdvSca1-SM cell reporter system, we discovered that AdvSca1-SM cells are major contributors to lung cancer progression and metastasis. While the role of cancer stem cells to cancer progression has been well established, the role of stromal progenitor/stem cells contributing to the tumor microenvironment and cancer progression and metastasis is a completely understudied area of research.