Contact UCHealth
Liver Cancer
Contact Children's Hospital CO
Clinical Trials
Make a Gift
What Is Liver Cancer?
The liver is the largest internal organ that lives in the upper right portion of the abdomen beneath the lung. The primary function of the liver is to regulate most chemical levels in the blood and excrete a product called bile. This helps carry away waste products from the liver.
Liver cancer starts when cells in the liver begin to grow out of control. The liver is made up mainly of cells called hepatocytes that can form cancerous and non-cancerous tumors.
Primary liver cancer forms in the liver and begins in the hepatocyte cells of the liver.
The most common type of primary liver cancer is called hepatocellular carcinoma. Secondary liver cancer, cancer that spreads, or metastasizes, to the liver from somewhere else in the body, is more common than primary liver cancer. Cancer that originates in another part of the body such as lung, esophagus, or colon then migrates to the liver is called liver metastasis or hepatic metastasis and is named for the organ in which it began.
According to the American Cancer Society, more than 41,630 new cases of primary liver cancer are diagnosed and there are an estimated 29,840 deaths from the disease each year. Primary liver cancer is more prevalent in men than women with an 8.3% higher incidence rate and a 5.7% higher death rate over women. Since 1980, liver cancer incidence rates have more than tripled and death rates have more than doubled.
In Colorado, there are an estimated 600 new cases and 420 deaths from primary liver cancer each year.
Liver cancer is much more common in countries in Southeast Asia and sub-Saharan Africa than in the United States. In many of these countries it is the most common type of cancer. Each year more than 800,000 people are diagnosed with liver cancer around the world. Liver cancer is also the leading cause of cancer deaths worldwide, accounting for more than 700,000 deaths each year.
Why Come to CU Cancer Center for Liver Cancer
CU Cancer Center doctors offer patients a comprehensive evaluation of benign and cancerous conditions of the liver. The CU Cancer Center is also one of four National Cancer Institute Designated Comprehensive Cancer Centers in the Rocky Mountain region. We have doctors who provide top-notch, multidisciplinary, patient-centered care and treatment options not available at most other medical centers in the country.
Our doctors are the only physicians in a 500-mile radius who are part of the National Comprehensive Cancer Network (NCCN) advisory panel. The NCCN establishes treatment guidelines that doctors all across the United States use as a reference.
There are over 100 liver cancer clinical trials, which includes several trials dedicated to the treatment of liver cancer, currently being offered by CU Cancer Center members, giving patients many different treatment options.
The Liver Multidisciplinary Clinic at the CU Cancer Center brings together a team of expert surgical oncologists, liver transplant surgeons, interventional radiologists, pathologists, medical oncologists, radiologists, radiation oncologists, and more to focus on problems affecting the liver. Together, the team analyzes a patient’s diagnosis and recommends a specific treatment plan for the individual by the end of the visit. Twenty to 30% of patients who are evaluated using a multidisciplinary approach have a change in their original diagnosis or treatment plan.
For more information on pediatric liver cancer, and to learn more about the care options and conditions treated, visit the pediatric Surgical Oncology Program and our Solid Tumor team at Children’s Hospital Colorado.
Our clinical partnership with UCHealth has produced survival rates higher than the state average for all stages of liver cancer.
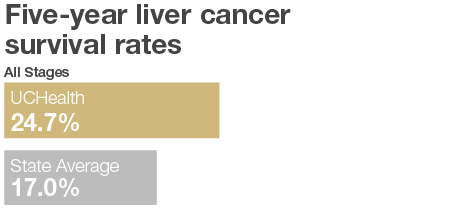
Number of Patients Diagnosed – UCHealth 1,800 – State of Colorado 8046
Number of Patients Surviving – UCHealth 436 – State of Colorado 1505
*n<30, 5 Year Survival – (Date of diagnosis 1/1/2010–12/31/2014)
Number of Patients Surviving – UCHealth 436 – State of Colorado 1505
*n<30, 5 Year Survival – (Date of diagnosis 1/1/2010–12/31/2014)
Types of Liver Cancer
There are two types of liver cancers, primary liver cancers, and secondary liver cancers.
The two most common forms of primary liver cancers are:
Hepatocellular carcinoma (HCC), the most common form of liver cancer in adults, can have different growth patterns. Some hepatocellular cancers start as a single tumor that grows slowly over time. Others start as many cellular nodules throughout the liver, not one single tumor.
Intrahepatic cholangiocarcinoma (bile duct cancer) starts in the cells that line the small bile ducts within the liver. Cholangiocarcinomas account for 10%-20% of cancers that start in the liver.
Secondary liver cancer is cancer that did not start in the liver but spread (metastasized) to the liver from another part of the body. Liver metastases, cancerous tumors that spread to the liver, commonly start as cancer in the colon or rectum.
Angiosarcoma and hemangiosarcoma are rare cancers that start in the cells that line the blood vessels of the liver. Fast growing tumors, angiosarcoma, and hemangiosarcoma are often treated with chemotherapy and radiation because they grow too quickly to be removed surgically.
In addition to treating all types of liver cancer, CU Cancer Center doctors are also experienced in treating a variety of benign (non-cancerous) liver tumors. Several types of tumors can form from the different types of cells that make up the liver. The
causes of these tumors vary and require different treatments. CU Cancer Center experts treat the following non-cancerous liver tumors:
Hemangioma are the most common benign liver tumor. Hemangiomas are abnormal blood vessels that don’t often cause symptoms but may bleed or cause pain.
Focal nodular hyperplasia, tumors that derive from several cell types, hepatocytes, bile ductules, and Kupffer cells, do not bleed or become cancerous but are commonly removed because they can grow very large, causing symptoms similar
to liver cancers.
Adenoma are benign hepatocyte tumors that can rupture and bleed and become cancerous. For this reason, they are commonly removed.
Cyst, a cavity in the liver that contains fluid that can become enlarged or infected and require removal.
Other tumor types that don’t typically require treatment include hamartomas, regenerative nodules, and lipomas.
Gallbladder cancer is abnormal cell growth in the small, pear-shaped organ that lives beneath the liver. Gallbladder cancer is a very uncommon cancer that often goes undiscovered until later stages. Because gallbladder cancer tends to migrate to the liver, the two require similar treatments. Aside from resection of the gallbladder and possibly a portion of the liver, this cancer can be treated with chemotherapy, radiation, targeted drugs, and immunotherapy.
Causes of Liver Cancer
Liver cancer is caused by DNA changes or mutations that occur within healthy cells. Normal cells in the body go through a life cycle where they grow and divide to form new cells and then die when the body no longer needs them. Cells contain DNA that tells the cell what to do. When a cell’s DNA is damaged, cells continue to grow and divide where they aren’t needed by the body. This buildup of cells becomes a tumor.
Certain chemicals can cause damage to the DNA in the liver cells and this damage can cause abnormal or mutated cells to grow. The hepatitis virus and chronic hepatitis infections are also known to cause liver cancer.
Risk Factors for Liver Cancer
There are several factors that might increase the chance of developing liver cancer. These risk factors include:
Gender: Hepatocellular carcinoma is more common in men than in women.
Race: Of all racial groups in the United States, Asian Americans and Pacific Islanders have the highest incidence rates of liver cancer.
Chronic viral hepatitis: Chronic infection with the hepatitis B virus (HBV) or hepatitis C virus (HCV) is the most common risk factor for liver cancer.
Cirrhosis: An irreversible condition that causes damage to liver cells and creates scar tissue. Cirrhosis is a progressive disease that increases the chances of developing liver cancer.
Weight: Non-alcoholic fatty liver disease is common among obese people. Non-alcoholic steatohepatitis, a subtype of this disease can cause cirrhosis and lead to an increased risk of liver cancer.
Inherited liver diseases: Hereditary hemochromatosis and Wilson’s disease can increase the risk of developing liver cancer.
Diabetes: People with diabetes have a greater risk of liver cancer than other people.
Excessive alcohol use: Alcohol abuse over many years can lead to irreversible liver damage linked with an increased risk of liver cancer.
Symptoms of Liver Cancer
Most people diagnosed with liver cancer develop symptoms in the later stages of the disease. Signs and symptoms of liver cancer include:
Unexplained weight loss: Many people who develop liver cancer notice unplanned weight loss due to loss of appetite.
Feeling full after a small meal: This is caused by an enlarged liver or spleen pushing against the stomach.
Nausea/vomiting: This can also include coughing up blood.
Pain or swelling in the abdomen: This is caused by swelling of the spleen or liver or fluid accumulation in the abdomen.
Jaundice: Also known as yellowing of the skin or eyes.
Diagnosing Liver Cancer
For high-risk patients, some liver cancers can be screened for before the development of symptoms. Exams, tests, and procedures to diagnose liver cancer include:
Blood tests: To check liver kidney and liver function, number of blood cells, and help diagnose cancer or other conditions, a blood test may be ordered. There are a number of different blood tests that can help identify liver cancer. These tests include:
- The alpha-fetoprotein blood test (AFP) looks for elevated levels of this protein. Elevated levels of AFP can sometimes indicate cancer is present.
- A liver function test (LFT) helps reveal liver function abnormalities which may lead to a liver cancer diagnosis.
- Blood clotting tests measures the levels of blood clotting factors to determine if the liver has been damaged. A low blood clotting factor count can lead to an increased risk of bleeding.
- Kidney function tests look at the blood urea nitrogen (BUN) and creatinine levels to determine how well the kidneys are functioning.
- A complete blood count (CBC) is a test that measures the levels of red blood cells, white blood cells, and platelets in the blood. Lower levels of red blood cells mean the bone marrow is not functioning properly, elevated levels of white blood cells mean there is an infection the body is trying to fight off, and a low platelet count means the blood has low clotting factors.
- A blood chemistry test checks the levels of calcium, glucose, and cholesterol which can all be affected by the presence of liver cancer.
Imaging tests: To look inside the body and help find suspicious looking areas of the liver, imaging tests like an ultrasound, CT scan, MRI scan, or angiogram may be ordered.
- Ultrasound is usually the first test to look at the liver and its condition. An ultrasound can show tumors forming in the liver.
- A CT scan uses x-rays to take detailed images of the body and can help identify several types of liver tumors. A CT scan can provide detailed information about the size, shape, and location of tumors in the liver.
- MRI scans use radio waves and magnets to take images of the body. MRIs can be used to look at the blood vessels in the liver to see blockages.
- An angiogram is an x-ray test that uses a dye injected into an artery to look at the blood vessels in the liver.
Biopsy: In some cases, to help make a definitive diagnosis, a small amount of liver tissue will be removed and tested in a laboratory for liver cancer. This procedure is called a biopsy and is conducted by inserting a needle into the liver to obtain the tissue sample. Note: not all patients with liver cancer require a biopsy. The three types of biopsies include:
- Needle biopsy is a procedure where a long hollow needle is inserted into the liver to remove a small amount of tissue.
- Laparoscopic biopsy is a procedure where a scope is used during a laparoscopy to remove tissue samples. The scope allows the doctor to see the surface of the liver to take specimens from abnormal-appearing areas.
- Surgical biopsy is done during surgery where either a portion of a tumor (incisional biopsy) or the entire tumor and some surrounding tissue (excisional biopsy) is removed.
Stages of Liver Cancer
The most commonly used staging system for liver cancer is the American Joint Committee on Cancer. The TNM system assesses the size and extent of the tumor (T-tumor), how large the tumor has grown, there are more than one; whether the cancer has spread to nearby lymph nodes (N-node); and the presence and extent of metastasis (M-metastasis) to distant lymph nodes and organs like the lungs.
Liver cancer is staged based on the results of tests performed like physical exams, biopsies, and imaging tests.
Liver Cancer Stages
Stage 1: A single tumor 2 cm or larger has formed in the liver but has not grown into the blood vessels or spread to nearby lymph nodes or distant sites.
Stage 2: A single tumor larger than 2 cm that has grown into the blood vessels, or more than one tumor smaller than 5 cm and has not yet spread to the lymph nodes or distant sites.
Stage 3: At least one tumor has grown into a vein of the liver or a tumor has spread to nearby lymph nodes but not distant sites.
Stage 4: A tumor or multiple tumors have spread to nearby lymph nodes and have possibly spread to distant organs such as the lungs.
These stages can be further broken down based on the size of the original tumor and the extent to which the cancer has spread.
Treatments for Liver Cancer
Treatment for liver cancer is tailored to each patient and is dependent on the stage of the cancer, where it is located, and other health concerns. Liver cancer care teams may include multiple health care specialists including surgical oncologists, liver transplant surgeons, interventional radiologists, pathologists, medical oncologists, radiologists, and radiation oncologists. Treatment of liver cancer mainly relies on the classification of whether or not the cancer is resectable.
Surgery for Liver Cancer
Full resection or removal of a liver tumor with a small portion of health tissue offers the most favorable outlook. A tumor’s resectability depends on the size and location in the liver, how well the liver functions, and the patient’s overall
health.
Partial hepatectomy is a procedure during which part of the liver is removed if the patient has good liver function and is healthy enough for surgery, usually stage I or stage II.
Liver transplant is an option for a small percentage of patients with tumors that cannot be removed surgically. During a liver transplant, the diseased liver is removed and replaced with a healthy donor liver.
Our experts are among the nation’s leaders in minimally invasive techniques for the surgical treatment of liver cancer. The minimally invasive approach involves inserting a camera and delicate surgical instruments into the body through multiple
small incisions instead of one large opening. Sometimes a surgical robot may be utilized to allow for more precision and flexibility than would be feasible with conventional surgical instruments. Recovery is typically faster and less painful
than with conventional surgery.
Localized Treatments for Liver Cancer
Ablation uses an electric current to destroy liver tumors without removing them. This procedure can only be performed on small tumors when surgery is not an effective option. Ablation is less likely to cure liver cancer than surgery.
- Radiofrequency ablation uses high-energy radio waves to heat up the tumor and kill the cancer cells.
- Microwave ablation uses electromagnetic waves to heat and kill cancer cells.
- Cryoablation uses liquid nitrogen to freeze and destroy cancer cells.
- Ethanol ablation is a procedure where concentrated alcohol is injected into the tumor to kill the cancer cells.
Embolization therapy is a procedure where a substance is injected into an artery in the liver to block the blood flow to a tumor, helping to kill off the cancer cells. During this procedure, the doctor will place a small tube into the blood vessels that
feed the tumor and inject micoroscopic beads directly into the tumor’s blood supply. The beads attack the tumor in two ways by reducing the blood supply and releasing radiation or chemotherapy. There are three types of embolization, these include:
transarterial chemoembolization (TACE), selective internal radiation therapy (SIRT), and Y-90.
- TACE is a kind of chemoembolization.
- SIRT is another term for radioembolization.
- Y-90 refers to a radioactive isotope called Yttrium-90, which fills the microscopic beads that are inserted into the tumor’s blood supply.
Hepatic Artery Infusion Pump
Hepatic arterial infusion therapy is a treatment for patients that have Colorectal Cancer that
has traveled to the liver. During this procedure, doctors connect a metal pump to a tube that goes into the hepatic artery to deliver chemotherapy directly to the tumor in the liver. The pump, a small programmable device, is implanted into the patient’s
abdomen close to the liver to allow the medication to flow from the pump directly into the liver through a catheter.
Radiation Therapy for Liver Cancer
Radiation is a treatment that uses high-energy rays or particles that destroy cancer cells and shrink tumors. Radiation is a good option for patients with severe damage to the liver from cirrhosis or hepatitis infections.
The most common radiation for liver cancer is external beam radiation therapy (EBRT). This is when the radiation is from a source outside the body, similar to an x-ray but with stronger radiation. The procedure is painless, with multiple treatments over several
weeks.
Stereotactic body radiation therapy (SBRT) is another radiation option that can help target the radiation to a specific area to avoid nearby healthy tissue. This precision allows for a higher level of radiation to be given and leads to fewer side effects.
Targeted Drug Therapy for Liver Cancer
Targeted drugs are used to target the changes in cells that cause cancer. There are many targeted drugs available for treating advanced liver cancer.
Sorafenib (Nexavar) and Lenvatinib (Lenvima) are drugs that can be used to treat liver cancer if surgery is not an option and the cancer has not spread to other organs. Sorafenib, a pill taken twice daily, can work better for people with liver cancer
caused by hepatitis C. Lenvatinib is a pill taken once daily.
Regorafenib (Stivarga) and cabozantinib (Cabometyx) are drugs that can be used to treat advanced liver cancer when other treatments are no longer effective.
Monoclonal antibodies are man-made antibodies designed to attack liver cancer tumor cells and affect the tumor’s ability to form new blood vessels to continue to grow. Bevacizumab (Avastin) is a monoclonal antibody that targets vascular endothelial
growth factor (VEGF) and is used along with immunotherapy. Ramucirumab (Cyramza) is a monoclonal antibody that targets VEGF on cells to help stop the formation of new blood vessels and can be used to treat advanced liver cancer.
Immunotherapy for Liver Cancer
Immunotherapy uses drugs to train the immune system to enhance the body’s ability to fight cancer. One of the most important characteristics of the immune system is its ability to recognize and avoid attacking the body's normal cells. To do this, it uses “checkpoint” proteins on immune cells. Cancer cells sometimes use these checkpoints to keep the immune system from attacking them. Drugs that target these checkpoints — called checkpoint inhibitors — can correct this.
PD-1 inhibitor is a checkpoint protein on T cells which, when attached to a PD-L1, another protein, tells the T cell to ignore the other cell.
Atezolizumab (Tecentriq) targets the PD-L1 protein by blocking the protein to boost the immune response against cancer cells.
Pembrolizumab (Keytruda) and Nivolumab (Opdivo) are drugs that targets PD-1 to help boost the immune response to cancer cells.
CTLA-4 inhibitor Ipilimumab (Yervoy) is a drug that boosts the immune response by blocking CTLA-4, a protein on T cells that helps keep them in check.
Immunotherapy is often reserved for patients with advanced liver cancer.
Chemotherapy for Liver Cancer
Chemotherapy is a treatment that uses drugs that travel through the bloodstream to reach cancer cells in most parts of the body. Unfortunately, chemo has not shown to have a great impact on liver cancer and is rarely used except in rare forms of liver cancer.
The University of Colorado (CU) Cancer Center partners with UCHealth, Children’s Hospital Colorado, and Rocky Mountain Regional VA to provide clinical care. Please make an appointment with one of our clinical partners to be seen by a CU Cancer Center doctor.
UCHealth Cancer Care - Anschutz Medical Campus
1665 Aurora Court Anschutz Cancer Pavilion
Aurora, CO 80045
720-848-0300
UCHealth Cherry Creek Medical Center
100 Cook Street
Denver, CO 80206
720-848-0000
UCHealth Cancer Center - Highlands Ranch
1500 Park Central Drive
Highlands Ranch, CO 80129
720-516-1100
UCHealth Lone Tree Medical Center
9548 Park Meadows Drive
Lone Tree, CO 80124
720-848-2200
Children's Hospital Colorado:
13123 East 16th Avenue
Aurora, CO 80045
720-777-6740
Rocky Mountain Regional VA Medical Center:
1700 North Wheeling Street
Aurora, CO 80045-7211
303-399-8020
Latest News from the CU Cancer Center
Loading items....
Information reviewed by Christopher Lieu, MD, in September 2022.