Primary RPLND
What is it?
Retroperitoneal Lymph Node Dissection (RPLND) is removal of the lymph nodes that exist in the back of the abdomen. Testicular cancer can commonly spread to this part of the body.
Some patients have either no signs of tumor spread or signs of limited spread to these lymph nodes. However, there may be features of the pathology from the orchiectomy or imaging that indicate a high risk of having tumor spread. In these patients, we may offer surgical removal of these lymph nodes to determine if they are involved by tumor.
If there is no spread of tumor to these lymph nodes, then you may not need to follow up with your physician as frequently. (However, regular follow-up is still very important and necessary.) Also, you should not need as many CT scans. If there is a small amount of tumor spread, you may be able to avoid chemotherapy or reduce the amount of chemotherapy that you need to cure the cancer.
This surgery can be done with a traditional 10-inch incision on the abdomen that allows us to have open exposure to perform surgery. This approach has the longest track record of success. We also offer a minimally-invasive approach (robotic RPLND) utilizing a robotic surgical system where the same procedure is performed via a series of small (1/2-inch) incisions. This allows us to use a camera and smaller instruments to do the same procedure inside the abdomen. This is a newer approach but accomplishes the same goals. The early results indicate that, in certain patients, a robotic RPLND can be as safe and effective as a traditional RPLND.
What are lymph nodes?
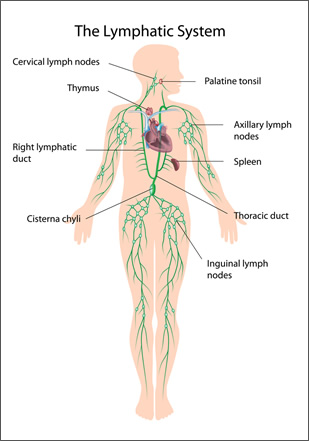
Lymph nodes exist all over body and are part of the immune system. Infections and cancers can spread to these areas. Lymph nodes can be safely removed with little long-term impact on overall health.
Every individual has a different number of lymph nodes that are removed during the surgery. Surgeons set anatomic boundaries and remove all the lymph-node tissue within those boundaries.
What are the possible complications of Retroperitoneal Lymph-Node Dissection?
Potential complications include:
- postoperative discomfort
- a risk of bleeding, as the operation occurs near some of the largest blood vessels in the body; however, a transfusion is needed in only about 10% of cases
- postoperative infections—these are rare but do sometimes occur. The most common type is a wound infection.
- With any cancer operation, the cancer can return after the surgery.
- Blood clots in the legs can occur after any major operation. This is one of the main reasons we encourage early mobility.
- A complication called chylous ascites can occur when fluid that would normally have been drained by the lymph nodes collects in the abdomen. This condition can persist for weeks or months. It is typically managed with drains or tubes; very rarely would it require further surgery to repair.
- There is a lifetime risk of a small-bowel obstruction. A small-bowel obstruction occurs when the intestines become blocked by scar tissue and material inside the intestine cannot pass through. This can result in abdominal bloating, pain, and vomiting. An obstruction of the small bowel can occur anytime after the surgery.
- A hernia or a bulge at the incision is a possibility as well.
- A common complication after this type of surgery is a loss of the ability to ejaculate. This occurs because the nerves that control ejaculation are in the area of the surgery and are commonly intimately involved with the tumors in this area. The surgery does not have any effect on the ability to obtain a penile erection nor the ability to experience sexual pleasure. Semen is produced but simply not ejaculated outward normally. (If desired, it can be collected and used for fertility.)
- Occasionally organs that are near the surgical site will be injured. These organs include the intestine, kidneys, ureters (the tubes which drain the kidneys), large blood vessels, nerves, pancreas, spleen, and liver. Occasionally, we will need to remove one or more of these organs as a part of the operation.
What happens if I have tumors in my abdomen and do not have surgery?
You may elect to have chemotherapy, which may be able to shrink or resolve these tumors. However, about 30 to 40% of the time there may be some tumor remaining after chemotherapy, which will require an RPLND after completing chemotherapy.
If left untreated by either surgery or chemotherapy, these tumors can enlarge, spread to other parts of the body, and cause pain or injury to nearby organs.
What can I expect after my surgery?
After surgery, patients will wake up with a catheter in their bladder. Occasionally a small drain is left inside the abdomen to drain excess fluid that may collect there. Patients will have their pain controlled with both intravenous and oral pain medications. Depending on the approach, there will either be an incision in the middle of the abdomen that is about 10 inches long or a series of 5-6 small (1/2-inch) incisions on the abdomen.
The day following surgery, we usually allow patients to drink and eat some small meals. Patients are allowed to walk in the hall of the hospital and are expected to sit up in a chair for several hours during the day. The catheter draining the bladder is usually removed on the second day after the surgery.
After robotic RPLND, many patients will leave the hospital two to three days after surgery. For a traditional RPLND, patients usually leave the hospital three or four days after the surgery.
It is not uncommon for patients to have poor appetite and energy level for several weeks. The important thing is to remain hydrated by drinking plenty of fluids. It may be recommended to follow a low-fat diet in the first few weeks after surgery to prevent leakage of fatty fluid (chylous ascites). Sleep patterns, eating habits, and bowel function will return to normal over a period of several weeks. We encourage patients not to lift any object heavier than 20 pounds for a month after the surgery. We would expect a return to pre-surgery levels by six weeks after surgery.
You will be provided with our clinic phone number should any problems arise. We will contact you once we know the pathologic results from the surgery if those are not back by the time you are discharged from the hospital.
We usually have a planned clinic visit four to six weeks after the surgery. At that time, we can review the findings from surgery and recheck your blood tests. This will allow us to come up with a personalized plan for your care going forward.