Peritoneal Dialysis Catheter Placement
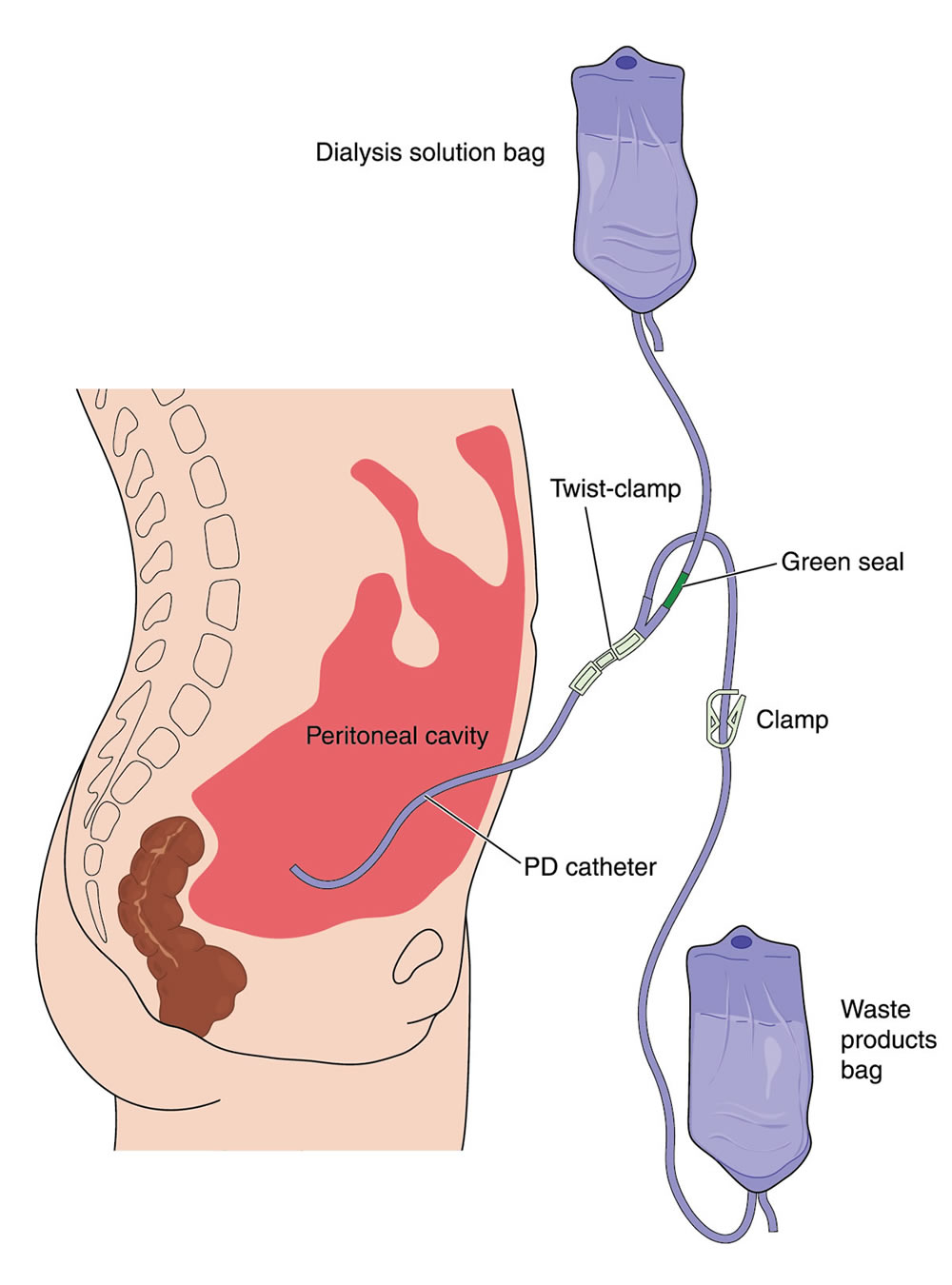
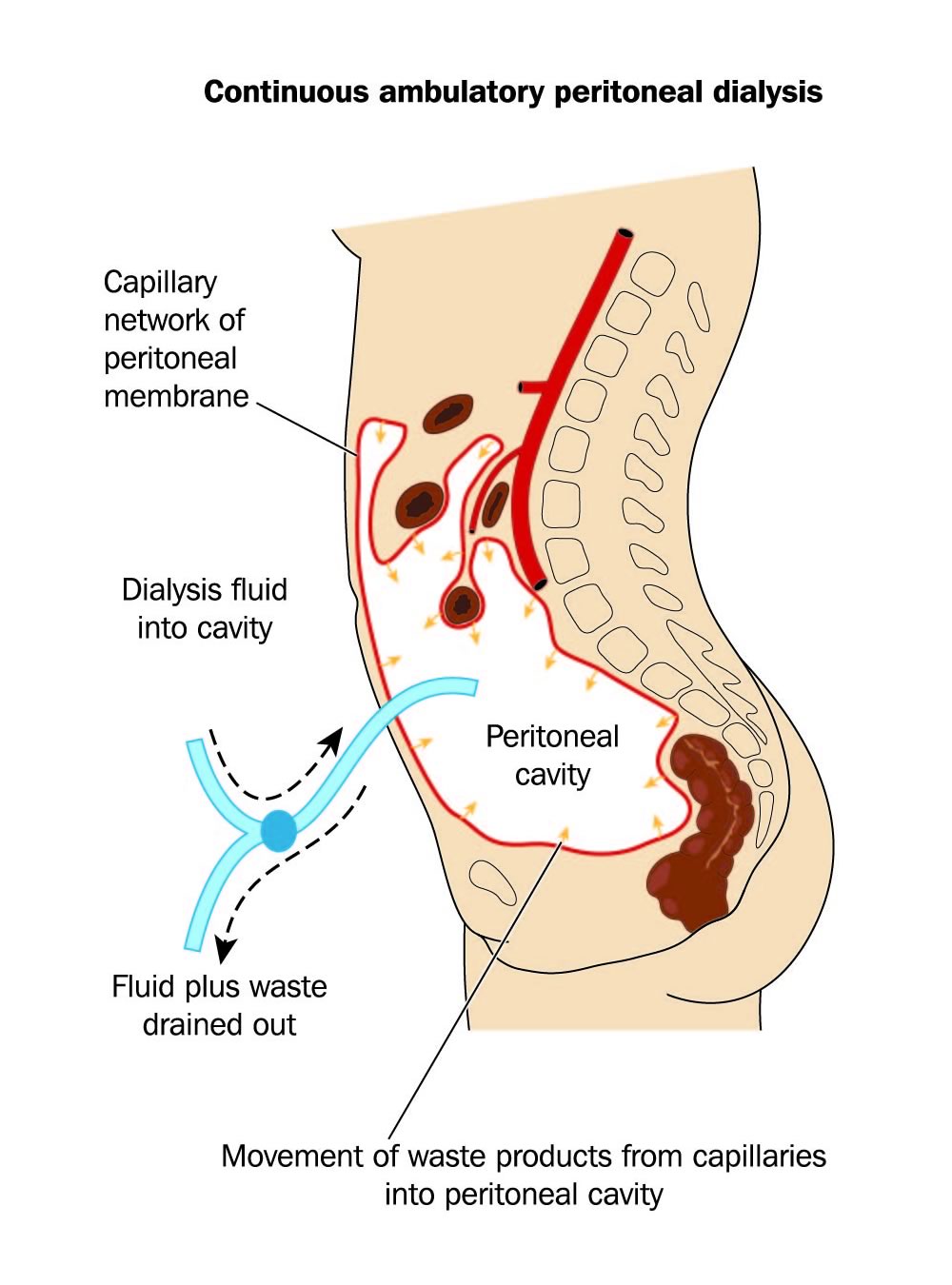
Some patients with end-stage renal disease are candidates for peritoneal dialysis, which uses the peritoneum as a filter to help remove toxins from the blood that can no longer be cleared by the poorly functioning kidneys. (The peritoneum is a thin membrane that lines the abdominal cavity and all the organs in the abdomen.) A catheter is placed in the abdominal cavity, permitting dialysis fluid to be instilled into, and then removed from, the abdomen.
Peritoneal dialysis catheters are placed under laparoscopic guidance by a surgeon. Laparoscopy, in which a camera is placed into the abdomen, allows the surgeon to view the structures in the abdomen to precisely place the catheter into the pelvis, and to free up any scar tissue that may have formed from any prior surgery or infection in the abdomen.
A peritoneal dialysis catheter offers the patient increased freedom and minimizes lifestyle interruptions. Once the catheter is surgically implanted, dialysis can be performed at home by the patient based on his/her individual schedule and needs. Dialysis can be performed either at night, with the aid of a machine called a “cycler,” or during the day, via manual exchanges. The cycler is portable and can even travel on an airplane. Additionally, supplies can easily be shipped to an alternate destination to allow patients to continue their dialysis while away from home. This process allows for much greater autonomy for patients than traditional hemodialysis. Patients will be teamed with peritoneal dialysis nurses who will train them on proper care and handling of the catheter, and will help maintain their peritoneal dialysis supplies.
The operation typically takes about one hour and is performed on an outpatient basis. Patients will require general anesthesia for the procedure. Patients can begin to use their new dialysis catheter as soon as the next day if needed. Before and after the surgery, there are some important instructions patients should follow to allow the catheter to continue to function properly. One of the most important is the use of stool softeners, which should be started 3 days leading up to the surgery and at least 3 days following the surgery. Patients should also make sure they do not have anything to eat or drink after midnight on the night before their operation. If patients take medications in the morning, they may do so with a small sip of water. See below for more specific guidance on these topics and recommended dosages of stool softeners.
Common Questions Regarding Peritoneal Dialysis Catheter Surgery
I was told to take stool softeners around the time of my surgery. Why?
It is very important to start taking a stool softener 3-4 days prior to surgery to help prevent constipation, and continue for 3-4 days after the procedure. Dr. Kennealey typically recommends taking Colace, 100mg 3 times per day. This medication is over-the-counter and does not require a prescription.
Constipation is problematic because it can prevent the the catheter from functioning properly. It can also make use of the catheter or flushing the catheter painful, and can even prevent the catheter from resting in its proper location in the pelvis. Undergoing general anesthesia and the use of pain medications post-operatively both cause constipation and will make existing constipation worse. Even if you feel you do not experience constipation, you should follow the regimen above to help ensure the best outcome after your surgery.
What do I need to do to prepare for my surgery?
- You should not have anything to eat or drink after midnight the night before your scheduled procedure. You may take medications as directed with a small sip of water only.
- Follow instructions given to you by your surgical team regarding the use of any blood thinning medications around the time of your surgery.
- Make sure someone accompanies you on the day of your surgery who can transport you home after you are discharged.
- Take stool softeners as directed above.
What should I expect following surgery?
Mild pain and discomfort after surgery are common. It’s normal to feel tired, experience a change in bowel pattern, or experience a loss of appetite following surgery. These symptoms should gradually resolve within a few days.
If you experience redness, swelling, increased abdominal pain, notice a foul smell or pus at the incision site, please call our office.
Please continue to take Colace (stool softener) 3 times per day while you are taking any narcotic pain medication.
Can I shower after surgery?
DO NOT shower until you have seen your Peritoneal Dialysis Nurse and he/she says it is okay to shower. It is important to keep the dressing dry.
When can I remove the dressing covering my catheter after surgery?
Please DO NOT remove the dressing covering your catheter. Your Peritoneal Dialysis Nurse will do this for you. The other small dressing can be removed 2 days after surgery.
When should I have my catheter flushed after surgery and when do I start Peritoneal Dialysis training?
Dr. Kennealey will call your nephrologist after surgery to let him/her know how the procedure went. Your nephrologist will arrange your first catheter flush and catheter care teaching with the peritoneal dialysis nursing team. In general, your catheter should be flushed at least every 7-10 days, or more frequently if possible, to maintain good functionality of the system.
Can I go swimming with a PD catheter?
You CANNOT go swimming after peritoneal dialysis catheter placement. Please discuss all questions related to swimming with your Peritoneal Dialysis Nurse
Do I need to come back to the clinic after my surgery?
Yes. You should be seen in the clinic 2-3 weeks after your surgery, where we will check your fistula and incision and remove any staples. Please call Kristin at 720-848-0833 to make your appointment.
Are there any restrictions after surgery?
No heavy lifting (anything over 20 pounds) for 3-4 weeks following surgery.