Autologous Tissue Reconstruction
Your plastic surgeon may offer you breast reconstruction using your own tissue (autologous reconstruction). Autologous breasts reconstruction consists of moving tissue (or flap) from one part of your body to reconstruct the breasts. There are two types of flaps that may be used, which are classified according to the attachment of the blood vessels.
The main benefits of autologous reconstruction are that in the majority of cases you do not need an implant, and the reconstructed breasts have a similar shape and feel of your native breasts. Another benefit is that the donor site will have a better contour since redundant tissue is removed. Disadvantages are that they are technically difficult, and there is a very small risk that the reconstruction fails (the tissue that was used to recreate the breasts does not survive).
Deep Inferior Epigastric Perforator (DIEP) Free Flap
Breast reconstruction using tissue from the abdomen provides one of the most natural results of all breast reconstruction options. DIEP flap consists of dissecting the abdominal tissue and the related blood vessels, moving the tissue to the chest, and reconnecting the blood vessels of the flap to the blood vessels of the chest wall to provide blood flow to the flap that will be used to create the new breast. There is a small amount of abdominal muscle and fascia that is opened at the time of harvesting to gain access to the vessels, but the muscle and fascia are preserved and closed after the harvest of the flap to minimize the risk of weakness and hernias in the abdominal wall. There will be a scar from hip bone to hip bone and another scar around the bellybutton.
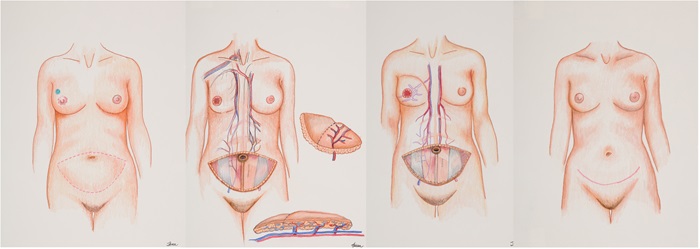
Superficial Inferior Epigastric Artery (SIEA) Free Flap
The free flap consists of abdominal skin, subcutaneous tissue and the associated superficial inferior epigastric artery and vein, and its perforators. Similar to the DIEP, the SIEA flap consists of dissecting the abdominal tissue and related blood vessels, moving the tissue to the chest and reconnecting the blood vessels of the flap to the blood vessels of the chest wall to provide blood flow to the flap that will be used to create the new breast. The SIEA free flap is not common as the caliber of these vessels is often too small. However, this option is used when these vessels are of adequate caliber because harvest of this flap does not require incision to the abdominal wall fascia and muscle. A decision to use this flap is usually made in the operating room. There will be a scar from hip bone to hip bone and another scar around the bellybutton.
Muscle Sparing TRAM (ms-TRAM) Free Flap
Depending on the size and availability of blood vessels, a flap may be created using skin, subcutaneous tissue and a small portion of muscle with or without fascia. Most of the muscle is spared, and otherwise the dissection is very similar to the DIEP flap. The vessels supplying the flap are disconnected from the abdomen like a DIEP flap and reconnected to the blood vessels of the chest wall to provide blood flow to the flap that will be used to create the new breast. There will be a scar from hip bone to hip bone and another scar around the bellybutton.
Latissimus Dorsi Myocutaneous Pedicled Flap
The latissimus dorsi myocutaneous flap is a flap from the back that is used for breast reconstruction. The latissimus dorsi muscle, along with the skin and fat that cover the muscle are elevated and moved to the front of your chest with the artery and vein still attached. Most women do not have enough fatty tissue on the back to re-create a breast so a tissue expander or an implant will also be used. The orientation of the scar is horizontally or slightly oblique on your back (the same side as the reconstructed breast). Your surgeon will usually attempt to hide the scar where your bra strap would typically lay.
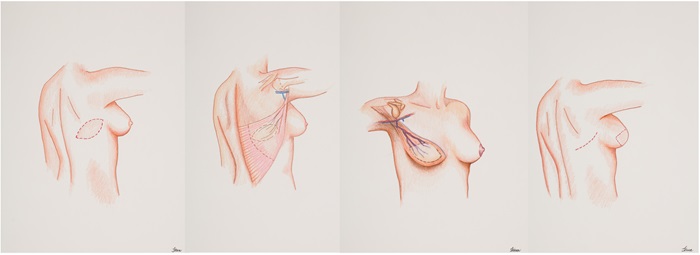
Benefits
- Decreased surgery and recovery time (versus free flaps).
- Bring healthy, non-radiated skin to the breast.
- Better coverage over the implant.
- Potentially one surgery required, if the implant is placed immediately.
Disadvantages
- Will likely require an implant for better volume and projection.
- Complications of the donor site such as collection of fluid or blood under the incision (seroma, hematoma) and scarring on the back.
- Muscle weakness in the back that affects active people, such as rock climbers, swimmers, and tennis players.
Transverse Upper Gracilis (TUG) Free Flap
Patients that desire autologous breast reconstruction but do not have adequate tissue from their abdomen may elect to use tissue from the inner thigh. The tissue consists of skin, fat and muscle and the underlying blood vessels in the region. The blood supply is from the gracilis muscle vessels that originate from the medial femoral circumflex system. The flap is dissected from the underlying tissue with its associated blood vessels and reconnected to the blood supply in the chest in order to provide blood flow to the flap that will be used to create the new breast. The gracilis muscle is located in the upper inner thigh. It starts at your pubic bone and ends along the inside of your upper leg. The gracilis muscle helps you bring your leg toward your body, but it is commonly used for various procedures and there is minimal functional loss from removing it. The main difference with the DUG flap is the orientation of the final scar. The orientation of the scar is horizontally in your upper inner thigh, and most surgeons will usually hide it in the crease of your thigh and buttocks.
Diagonal Upper Gracilis (DUG) Free Flap
Similar to the TUG flap, the DUG flap uses a patient’s own tissue from the inner thigh to create a new breast after a mastectomy. The free flap consists of skin, fat, and muscle along with the accompanying blood vessels. The blood supply is from the gracilis muscle vessels that originate from the medial femoral circumflex system. The flap is dissected from the underlying tissue with its associated blood vessels and reconnected to the blood supply in the chest in order to provide blood flow to the flap that will be used to create the new breast. There is minimal functional loss from removing the gracilis muscle. The main difference with the TUG flap is the orientation of the final scar. The orientation of the scar is diagonally in your upper inner thigh.
Profunda Artery Perforator (PAP) Free Flap
Patients that desire autologous breast reconstruction but do not have adequate tissue from their abdomen may elect to use tissue from the inner thigh. The tissue consists of skin and fat from the upper medial and posterior thigh. The blood supply is from the profundal femoris vessels. The flaps are dissected from the underlying tissue with their associated blood vessels and reconnected to the blood supply in the chest to provide blood flow to the flap that will be used to create the new breast. There is no muscle taken with this flap. The orientation of the scar is horizontally in your upper inner thigh, and most surgeons will usually hide it in the crease of your thigh and buttocks.
Superior or Inferior Gluteal Artery Perforator (SGAP or IGAP) Free Flap
Patients that do not have adequate tissue from their abdomen to perform autologous breast reconstruction may elect to use tissue from the buttock. The tissue consists of fat taken from the buttock region including the skin, fatty tissue and the underlying blood vessels. Flap is taken from the upper portion of the buttock which is supplied by the superior or inferior gluteal vessels. The flap is dissected from the underlying tissue with its associated blood vessels and reconnected to the blood supply in the chest to provide blood flow to the flap that will be used to create the new breast. The scar will be placed on the lower back just above the upper buttock.