Patient Care
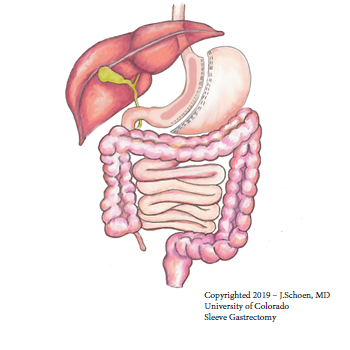
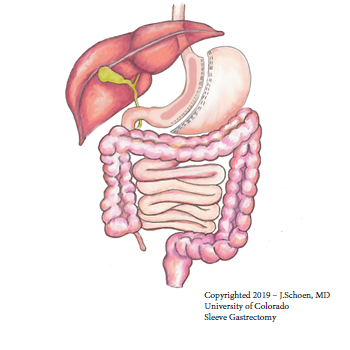
This procedure began as the first stage of a bariatric surgery called biliopancreatic diversion. This surgery had two stages. The sleeve gastrectomy reduced the patient's surgical risks for the second stage of the surgery by promoting significant weight loss. Because many patients were very successful with weight loss after undergoing sleeve gastrectomy, they decided with their surgeons to not have the second stage of the surgery.
How does the laparoscopic sleeve gastrectomy work?
A sleeve gastrectomy creates a small "sleeve" of a stomach that looks like a tube or a banana. This surgery removes about 80% of the stomach. As you would expect, patients lose weight by limiting how much food they can take in. It is also thought to contribute to weight loss by removing the part of the stomach that make grehlin, a hormone responsible for appetite.
Most patients will lose 50% of their excess body weight in the first year. No data is yet available for five-year outcomes. Therefore, doctors still consider this an experimental procedure since they do not really know how the surgery works for long-term weight loss and maintenance. However, available studies show that weight loss remains stable after the first year.
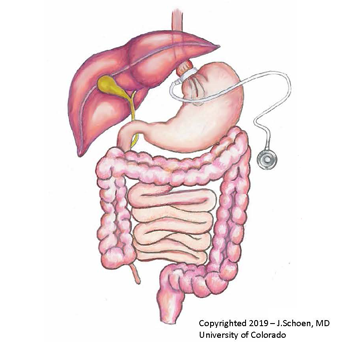
Laparoscopic Adjustable Banding (LAP-BAND) is the most common surgery for obesity in Australia and Europe. It has been in use in these countries since 1993. The United States FDA granted approval of the LAP-BAND in 2001.
Recent studies show that patients lose 30-40% of their excess weight (average weight loss) in the first two years after surgery. Weight loss slowly progresses to 50% of excess weight being lost at three years after surgery.
Most people maintain this weight loss over five years. However, up to 20% of patients with LAP-BAND surgery fail long-term weight loss.
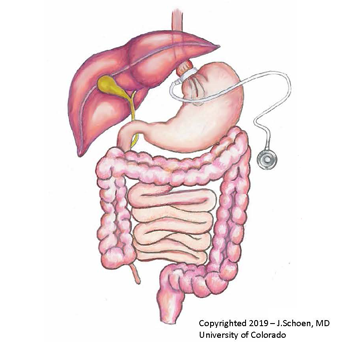
What is LAP-BAND?
The LAP-BAND is a silicone adjustable device. The surgeon, using laparoscopic (minimally-invasive) surgery, wraps this around the upper portion of the stomach. The patient is under general anesthesia (completely asleep). The band connects to a reservoir tube and port that lies on the abdominal wall muscle. The port cannot be seen, but it can be felt from the outside. The port and reservoir tube allows for adjustments to the LAP-BAND.
During the first year post-op, you will return to clinic several times to have this reservoir filled or deflated depending on your weight loss. Filling the port requires an injection of saline through the skin of the abdomen into the port.
How does LAP-BAND cause weight loss?
The placement of the LAP-BAND creates a small stomach pouch. This connects to the rest of the stomach by a small outlet (stoma). This results in a restriction in food intake. You can only eat small portions of food after LAP-BAND placement. You also stay full for longer periods of time as the food travels slowly through the stoma. This causes you to lose weight. In turn, you may also resolve or improve other illnesses related to obesity such as diabetes and high blood pressure.
The Roux-en-Y gastric bypass is the "gold standard" for the surgical treatment of obesity. It is well proven to be safe and effective.
In this procedure, your UCH surgeon uses a laparoscopic (minimally invasive) technique that allows placement of a tiny camera and micro instruments through five small incisions made in your abdomen. The surgeon creates a "new," smaller stomach and re-routes the digestive channel. With a smaller stomach, you will only be able to eat small amounts of food at one time.
What are the benefits of this approach?
Typically, minimally invasive surgical techniques:
- Decrease your time spent in the hospital (most patients leave after two days).
- Decrease your pain after the surgery.
- Reduce the chance of wound infections and abdominal wall hernias.
In rare cases, your surgeon may decide to perform an open gastric bypass, or convert to an open procedure during the middle of the operation. This is usually due to not being able to see the organs well enough with the laparoscope.
Other potential benefits of this surgery include:
- Greater mobility.
- Increased fertility.
- Decreased pressure on the joints.
- Improved self esteem.
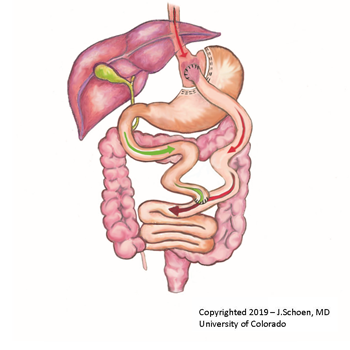
How does this surgery work?
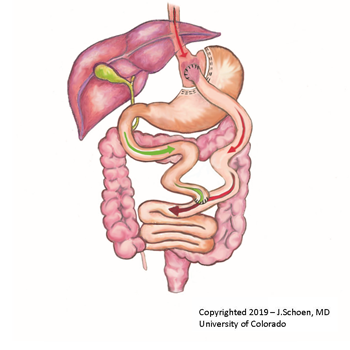
The surgery begins with the creation of a one-ounce gastric pouch, which will be your “new” stomach. This is the restrictive part of gastric bypass surgery.
Next, the small intestine is followed down about a foot and divided in two. The first portion is the “biliopancreatic limb.” The second portion, also called the “Roux limb,” is connected directly to your gastric pouch, bypassing the first part of your small intestine and “old” (excluded) stomach. This is the malabsorptive part of surgery.
Finally, the Roux limb and the bypassed section of the small intestine are connected to create a Y-shaped junction. The stomach remnant continues to produce the necessary juices for digestion. These juices, along with other enzymes and bile, flow through the bypassed intestine to combine with food at the biliopancreatic limb. Digestion and absorption occur from the “Y” point forward.
The Roux-en-Y gastric bypass produces weight loss by three mechanisms:
- Restriction: The stomach volume is much smaller after the surgery. Your stomach can only hold about one ounce, or 30 ml. You will only be able to take in small portions of food at any one time. For reference, the stomach can normally hold 67 ounces (about two quarts or liters).
- Malabsorption: After surgery, about 100 centimeters, or 40 inches, of bowel are excluded from digestion (bypassed). This area is no longer able to absorb calories, macronutrients, and vitamins. That is why it is so important that you take multivitamins every day for the rest of your life following the surgery. It is also important to monitor your nutritional status with yearly blood tests. There is still plenty of bowel for digestion. Some of the food that you eat does get absorbed further along in the small bowel, making it possible to “cheat” by eating high-caloric foods.
- Behavioral: About 70% of patients experience "dumping syndrome" following surgery. Patients experience symptoms such as abdominal cramping, nausea, diarrhea, sweating, and increased heart rate after eating high-sugar foods, or sometimes fatty foods. This is actually a desirable outcome as it usually serves as negative reinforcement and patients learn to avoid eating such foods.
An effective and lasting weight loss
Most studies show that patients lose an average of 60 to 70% of their excess body weight in the first year after Roux-en-Y gastric bypass surgery. They also are able to maintain that loss after several years of follow up.
In addition, a majority of patients with diabetes have complete remission of their disease. Most patients see improvements in other medical problems in the first few months following the procedure.
Remember, though, that your surgery is only a TOOL to help you achieve your weight-loss goals. Your surgery needs to be one part of a complete lifestyle change that emphasizes daily exercise and healthy eating habits that are tailored to your new anatomy.